Better safe than sorry with cancer screening
According to the WHO, cancer is globally the second leading cause of deaths
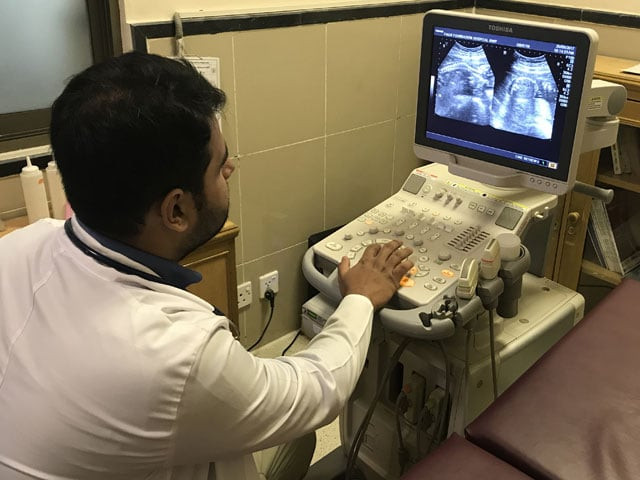
A doctor busy on an ultrasound device. PHOTO: RAJA KHALID SHABBIR
The word cancer was introduced by the Greek physician Hippocrates who used the term carcinos and carcinoma to describe non-ulcerating and ulcerating tumours. Cancer literally means a crab owing to the finger-like projections, more formally known as spiculations, seen mostly in the radiographic and microscopic analysis of breast tumours.
Promising drugs stoke talk of eventual cancer "cure"
Evidence from ancient manuscript and fossilised bones of human mummies in Egypt suggests an ardent relationship between cancer and humans. Tissue growths indicative of osteosarcoma (bone cancer) and skull destruction as seen in cancer of the head and neck have been found.
According to the World Health Organisation (WHO), cancer is globally the second leading cause of deaths and nearly every one in six deaths is due to cancer. However, one of the most viable options for controlling these figures is by introducing the judicious use of cancer screening in the worldwide medical lexicon.
 An MRI machine. PHOTO: RAJA KHALID SHABBIR
An MRI machine. PHOTO: RAJA KHALID SHABBIROften, we find ourselves pre-empting unwanted situations from happening in our routine lives, like locking doors every night to avoid any unforeseen event. Unfortunately, this concept of cautiousness falls short of achieving its due pragmatic importance when applied to disease prevention.
“Prevention indubitably is better than cure, in reality, it is the best cure. However, if prevention is not possible then early detection of disease and seeking early medical advice is of prime importance. This becomes even more important for a disease like cancer, which can grow to metastasize and become incurable within days to weeks. Owing to this fact, many screening programmes are run worldwide for different types of cancers,” says Dr Muhammad Sohaib Nadeem, Consultant Oncologist at Combined Military Hospital (CMH) Rawalpindi.
According to Dr Nadeem, “There are programmes for the general public (universal screening or mass population screening) and for high-risk individuals (selective screening) with specific cancers. The screening programmes for the general public include breast, lung, prostate and cervical (uterine cervix) cancer.”
Experts call for countrywide cancer database
Nevertheless, this approach is associated with limitations such as having adequate resources to conduct tests on a wide range of the population.
Screening programmes for high-risk individuals include screening for hepatocellular carcinoma (liver cancer) in hepatitis B or C positive individuals.
Cancer screening involves a wide range of techniques starting from a detailed history and physical examination to recognise warning signs and symptoms such as a lump, weight loss, chronic hoarseness, persistent indigestion, resistant sores, abnormal bleeding etc. Laboratory testing of blood and urine further also aids the process. Medical imaging such as ultrasonography, MRI and CT scan is used to detect the spread of the disease while mammography (X-ray image of the breast) is to locate breast tumours.
 An oncology (cancer) ward. PHOTO: RAJA KHALID SHABBIR
An oncology (cancer) ward. PHOTO: RAJA KHALID SHABBIRMeanwhile, gene testing for mutation while biopsy and endoscopy, which involves introducing a tubular instrument into the gut with a camera at the end, forms the invasive category of screening tests.
Now there are certain pre-requisites before taking on the screening pathway that includes effectiveness, specificity, availability of resources (personnel, equipment, etc.), acceptability, high prevalence of the disease to justify the efforts and cost of conducting the tests and facilities to confirm diagnosis and for subsequent treatment and follow-up of those with abnormal results.
The United States Preventive Services Task force, a group of national experts in prevention and evidence-based medicine, completely ignores the question of money. Most others, however, give preference to less expensive tests over expensive ones.
New cancer treatment boosts morale of terminally ill patients
Highlighting the reasons Dr Nadeem says, “Screening tests must be more sensitive than specific and must be cost-effective as we have to screen mass population. For a country like ours [Pakistan] with less available resources for health and huge population, cost-effectiveness becomes even more important. Specific confirmatory tests have to be done on very less number of patients.”
It is important to know that a doctor advising a screening test does not necessarily mean that you might have cancer. Screening tests are carried out on an apparently healthy target group to identify those having the disease. The aim of these measures is prevention and early detection of cancer. In addition, early detection of the disease by screening tests is a silver lining in the backdrop of the grim diagnosis as it improves the chances of recovery.
However, in Pakistan’s peculiar environment, patients usually visit hospitals when the disease has already entered the advanced stages, as indicated by metastasis to lungs, liver bone or brain, making treatment a huge challenge.
 A nurse preparing chemotherapy medication. PHOTO: RAJA KHALID SHABBIR
A nurse preparing chemotherapy medication. PHOTO: RAJA KHALID SHABBIRThe diagnosis of a disease that will never cause any symptoms or death during a patient's ordinarily expected lifetime is called over-diagnosis.
“Most of the cancers progress rapidly and then the early diagnosis is the key to save lives,” insists Dr Nadeem.
The term over-diagnosis can be applied in very elderly or frail patients with very slow-growing tumours. Yet over-diagnosis will not lead to the death of the patient. For instance in prostate cancer, is the screening is done, we shall be able to diagnose both slow-growing and fast-growing prostate cancers.
12 ways to staying cancer-free
“Fast-growing [prostate cancers] will be treated while slow-growing [prostate cancers] will be put on active surveillance. So no over the treatment of patients with slow-growing tumours will be required but patients with fast-growing tumours will be diagnosed early and treated before reaching a metastatic or untreatable condition,” explains Dr Nadeem.
Some screening procedures due to their invasive nature are close to a double-edged sword. Therefore, the benefits should clearly outweigh the harms and the medical indications should be distinct before undertaking any such procedure.
Colonoscopy and sigmoidoscopy, which detect colon cancer, involves inserting a tube with a camera at the end into the large intestines that might cause tears and bleeding.
Some imaging modalities like X-rays and CT scans use harmful ionising radiations, which can, unfortunately, develop into new cancer.
Screening mammography, a test to detect breast cancer is not very useful in young females because, at a young age, breast tissues remain dense which hampers the screening capability of the test.
 PHOTO: RAJA KHALID SHABBIR
PHOTO: RAJA KHALID SHABBIROther risks include abnormal results when in reality the patient has no cancer and normal results when in fact the patient has the disease. This is referred to as a false-positive or false-negative result respectively. False-positives can lead to needless medical procedures such as taking a biopsy, which involved needle pricks, to confirm the diagnosis while false-negatives prevent further diagnostic evaluation and treatment, leading to unnoticed progression of the disease.
Notwithstanding the above-mentioned risks, cancer screening also has other complexities such as misdiagnosis most commonly between lung cancer and tuberculosis.
Chemotherapy may spread cancer, warn scientists
According to Dr Nadeem, “As tuberculosis is prevalent in our part of the world, doctors even pulmonologists at times tend to treat patients having symptoms or radiological findings of lung cancer, as cases of tuberculosis. When patients do not respond to one or two lines of anti-tuberculosis drugs, the physician then starts thinking of some other diagnosis. This leads to delay in lung cancer diagnosis. Meanwhile, cancer spreads and reaches the incurable and sometimes unmanageable stage.”
Now, there are varying opinions about laying-off cancer diagnosis of a patient having low life expectancy due to a chronic disease, for instance, end-stage renal disease.
“No one knows whether he [patient] will die of a chronic disease or some recently acquired acute disorder. Therefore, diagnosis and treatment of any disease is necessary. Secondly, no one can predict how aggressive cancer would be and how much misery and morbidity it will add to the chronic ailment. So knowing it early will help reduce misery and add to the quality of life. Even if we cannot add days to life still we can add life to days,” adds Dr Nadeem.
The American Cancer Society has put forth some preventive steps to help reduce cancer risks. Staying away from all forms of tobacco, doing regular physical activity, eating plenty of fruits and vegetables, achieving ideal body mass index (BMI), limiting alcohol intake, protecting skin from the sun’s harmful ultraviolet rays, knowing your family history and getting regular check-ups and cancer screening tests are some of those steps.
 PHOTO: RAJA KHALID SHABBIR
PHOTO: RAJA KHALID SHABBIRScreening guidelines
Breast Cancer: This cancer before the age of 20 is rare but the incidence increases with age. For breast cancer, a combination of clinical assessment, radiological imaging and a tissue sample for histological analysis is used. This is called triple assessment. The imaging modalities include ultrasonography and mammography while a biopsy is done later to confirm its diagnosis. Mammography is an extremely safe investigation as it uses low-voltage, high-amperage X-rays with a small radiation dose. Its sensitivity rises with age as the breast tissue becomes less dense. For younger women, instead of a mammogram, ultrasound is preferred. Breast MRI is also done in specific settings. The least invasive, rapid and most accurate technique of taking a biopsy is fine needle aspiration cytology (FNAC).
Chemotherapy may spread cancer, warn scientists
Prostate Cancer: This is the most common malignant tumour in men over the age of 65. The cancer detection rate using PSA (prostate-specific antigen) measurements is between 2-4 per cent. Some 20 per cent men with clinically significant prostate cancer will have PSA levels within the normal range. Therefore, PSA alone as a screening test is controversial. If digital rectal examination reveals a prostate that is hard and nodular accompanied with high PSA levels, then trans-rectal ultrasound scan (TRUS) and biopsy are indicated. MRI and TRUS are for staging local disease. While x-ray of chest and liver function tests are carried out for metastatic spread of the disease.
Colorectal Cancer: This cancer typically occurs after 50 and is most common in the eighth decade of life. A digital rectal exam is done for rectal carcinoma. Endoscopy, which consists of a camera attached to a flexible tube, is done to visualise the colon and rectum and a biopsy may be taken from any suspected area or mass. Double contrast barium enema, CT scan, chest X-ray and liver ultrasound are used to check the extent of the disease.
The significance of cancer screening can also be gauged by an interesting story of Ben Stiller – a US actor and comedian famed for his role in the Night at the Museum movie series – who was diagnosed with having prostate cancer in June 2014. Having no symptoms or positive family history, Stiller published an essay on Medium about his ordeal, suggested a painless blood test to check PSA (Prostate Specific Antigen) levels. Fortunately, the silent disease was caught in early stages and treated.
Even after being cured, why you think people continue to get tests they do not need and that may exact costs to their health and time. Because it is better to be safe than sorry. What is the need of taking chances that a possibly lethal cancer will go unnoticed until it is too late for a treatment? Something is always better than doing nothing.
Raja Khalid Shabbir is a doctor and freelance writer based in Islamabad. He can be reached at @rajakhalidshab.



















COMMENTS
Comments are moderated and generally will be posted if they are on-topic and not abusive.
For more information, please see our Comments FAQ