Nocturnal enuresis: Don’t dampen your spirit
Nocturnal enuresis may hinder a good night’s sleep but can easily be managed
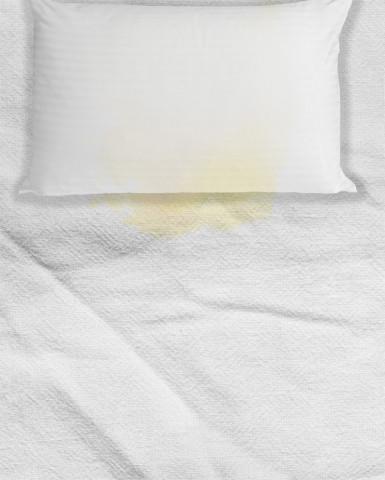
Nocturnal enuresis may hinder a good night’s sleep but can easily be managed. DESIGN: ESSA MALIK
The condition is classified into two categories:
1. Primary NE is the recurrent involuntary bedwetting by a child aged five years or older, who has never achieved bladder control and consistent nighttime dryness. It has a prevalence rate of around 9% in children between the ages of 5-10
2. Secondary NE is the involuntary bedwetting by a child who has been dry at night for at least six months. Secondary NE only forms 5-10% of all cases and is usually triggered by an underlying stressor.
Effects:
Nearly all children with bedwetting report a perceived sense of helplessness and hopelessness as they feel unable to control their condition while most other children are able to stay dry at night. Some parents also report psychological consequences in children such as low self-esteem, poor socialisation, anger issues and behavioural problems.
Management:
The management of secondary NE involves addressing the underlying stressor if one can be identified. Most children with secondary NE, however, have no identifiable cause and are treated in the same manner as children with primary NE.
Parents can do the following to help their child overcome the condition:
1. Reassure the child that NE is nothing to be ashamed about; that it is a part of normal development and will subside in time
2. Limit the amount of fluid ingested especially before going to bed.
3. Limit the amount of beverages, caffeine and sweets consumed by the child.
4. Ensure that the child uses the toilet before going to bed and also has access to one during the night.
5. Wake the child up after every four hours throughout the night to use the toilet. This is to sensitise the bladder and ensure that the child develops the habit of waking up to relieve themselves.
6. Motivate the child by rewarding them for staying dry and making star charts to mark dry nights.
7. Use specialised mattresses and alarms if needed.
Causes:
— The most common cause for bedwetting is a simple delay in the child’s ability to stay dry while having no other developmental issues.
— There is a higher incidence of cases in children with a family history of primary NE.
— The body normally produces a higher level of Anti-diuretic hormone (ADH) at night, signaling the kidneys to produce less urine. If the body’s ADH response is inadequate, it leads to excessive urine production often beyond the capacity of a child’s bladder. ADH levels usually normalise around the age of 10.
— Urinary tract infections, neurological problems, diabetes, constipation and child abuse (emotional or physical) are also common causes of secondary NE.
Saadia Khan is a pediatric resident from Multan. She tweets @drkhanchc
Published in The Express Tribune, Sunday Magazine, January 18th, 2015.



















COMMENTS
Comments are moderated and generally will be posted if they are on-topic and not abusive.
For more information, please see our Comments FAQ