According to the World Health Organization, over 422 million people are affected by diabetes worldwide, making it one of the most critical health issues today. Despite its prevalence, diabetes remains surrounded by myths and misunderstandings.
On this World Diabetes Day, with the theme “Breaking Barriers, Bridging Gaps,” the focus is on ensuring that everyone has access to empowering diabetes care. Diabetes management doesn’t have to be complex—with the right support and tools, anyone can gain control over their health.
To address some of the most common questions about diabetes, we’ve gathered 10 of the most frequently asked questions on diabetes, aiming to support you on a journey to better health.
1. How many types of diabetes are there?
Diabetes mainly falls into three categories: Type 1, Type 2, and gestational diabetes. Type 1 is an autoimmune condition often diagnosed in younger individuals, requiring insulin injections as their bodies can’t produce insulin. Type 2, typically influenced by lifestyle factors, develops gradually and is often manageable through lifestyle adjustments. Gestational diabetes occurs during pregnancy due to hormonal changes and can raise the mother’s future risk of developing Type 2 diabetes. Understanding the type of diabetes is essential, as each requires a unique approach to management.
2. What causes diabetes?
Diabetes is often linked to genetics and lifestyle factors. Environmental and genetic triggers can provoke an autoimmune reaction causing Type 1 diabetes. In Type 2 diabetes, lifestyle choices—like diet and exercise—along with genetic factors play a significant role. A family history of diabetes increases the risk, but it's not inevitable. For Type 2, healthier lifestyle choices, such as a balanced diet and regular physical activity, can help prevent or delay onset.
3. How can I tell if I have diabetes?
Signs of diabetes include frequent thirst, excessive urination, fatigue, blurred vision, and unexplained weight loss. If you notice these symptoms, consult a doctor. A simple blood test can confirm diabetes. Early diagnosis often surprises people by how manageable diabetes can be, so don’t delay if you experience these warning signs.
4. Is diabetes reversible?
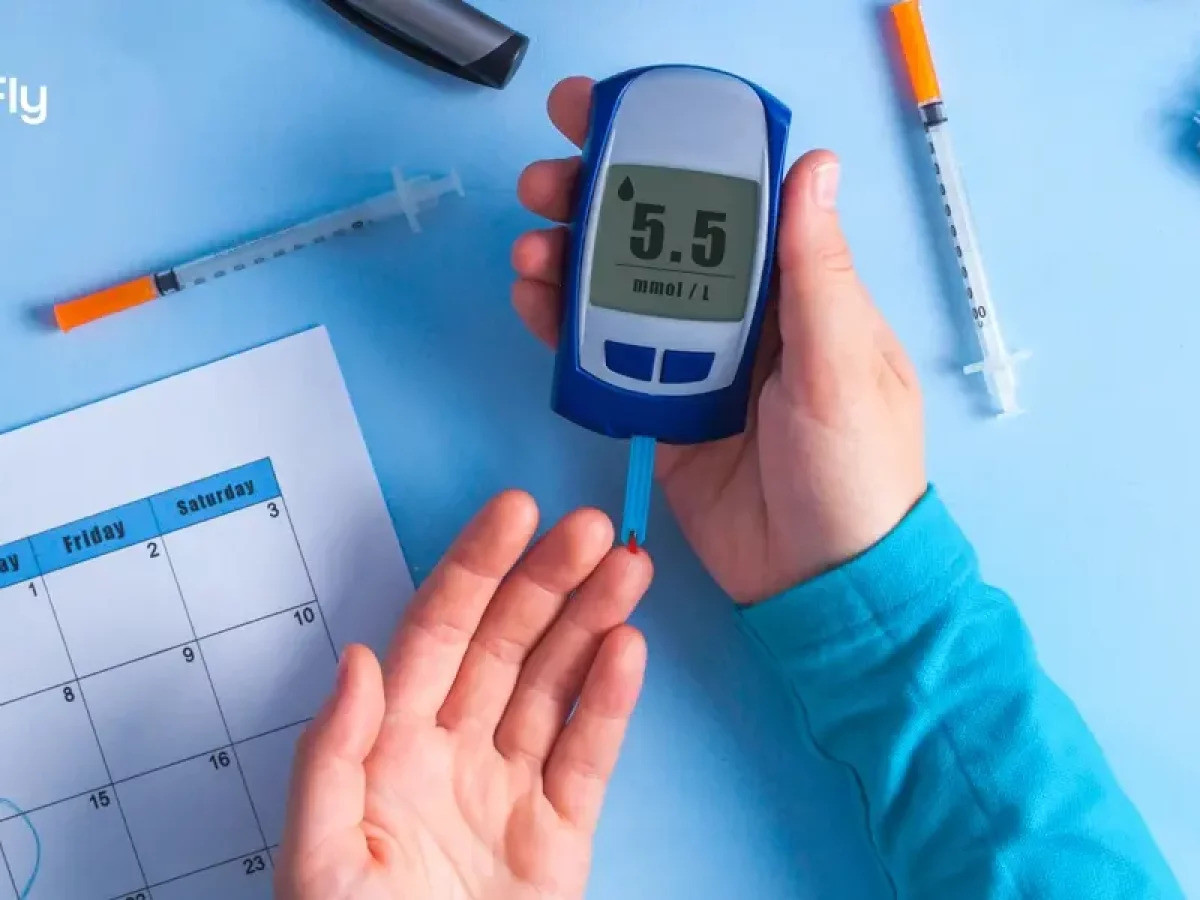
Currently, diabetes has no cure, but it is manageable. With tools like blood sugar monitoring and dietary changes, living a long, healthy life with diabetes is achievable. Although researchers are working toward a cure, especially for Type 1, the current goal is effective management.
5. How can I control my blood sugar?
Managing blood sugar requires consistency and balance. A healthy diet, regular exercise, and frequent monitoring are key. Simple changes—like reducing sugary drinks or opting for whole grains—can significantly impact. Tracking your levels helps you understand the effects of these changes over time. Technology, such as smart glucometers and personalized insights, offers additional support, helping you track health metrics and access expert advice.
6. What foods should I eat if I have diabetes?

Focus on foods that maintain steady blood sugar levels, like vegetables, whole grains, and lean proteins. A balanced meal with carbs, proteins, and fats is ideal. Eating smaller, frequent meals also helps keep blood sugar stable. Since individual needs vary, consider consulting a nutritionist to find what works best for you.
7. Can people with diabetes exercise?
Absolutely. Exercise is one of the best ways to help the body use insulin more efficiently and regulate blood sugar. Begin with low-impact activities like walking or cycling, and monitor your blood sugar before and after to ensure safety, especially if using insulin.
8. How does diabetes affect mental health?
Living with diabetes can feel overwhelming, leading to stress or even burnout. Creating a manageable routine and talking with support groups, friends, or family can help. Self-compassion is vital—it’s a marathon, not a sprint.
9. What complications are associated with diabetes?
If uncontrolled, diabetes can lead to heart disease, kidney issues, nerve damage, and vision problems. Regular checkups and blood sugar management can often prevent these complications. Proactive health screenings for your heart, kidneys, and eyes can help detect and manage potential issues early.
10. Can Type 2 diabetes be prevented?
In many cases, yes. Eating a healthy diet, regular exercise, and maintaining a healthy weight can reduce your risk. Small daily choices—like drinking water over sugary beverages or choosing stairs over elevators—make a big difference. Routine checkups also help by identifying early signs, allowing you to make adjustments before diabetes develops.
Managing diabetes is all about consistency—taking small steps each day toward better health, rather than striving for perfection. This World Diabetes Day, let’s remember that every positive change counts, and no one has to manage diabetes alone.








COMMENTS (2)
Comments are moderated and generally will be posted if they are on-topic and not abusive.
For more information, please see our Comments FAQ