Little to worry about, but Pakistan remains alert
Ports of entry across the country heighten surveillance after first case
For the second time in two years, the World Health Organization has declared a global emergency over the rapidly spreading mpox outbreak. Just two days after this latest alert was issued, Pakistan's health ministry confirmed the country's first mpox case in a returning traveler from a Gulf country.
As the case was still being sequenced and the variant remained unclear, authorities in Khyber Pakhtunkhwa (K-P) allowed the young male to return to his hometown of Mardan. Initial media reports, citing the district health officer, indicated that the patient had traveled to Dir, 240 kilometers from the provincial capital, but has since returned and is now quarantined at home.
But a day before authorities in northern Pakistan raised the alarm, Sweden confirmed its first case of mpox clade I, a more dangerous variant of the disease – suggesting that the virus had already slipped out of the Democratic Republic of Congo, where it has been spreading like wildfire and has caused more than 500 deaths to date.
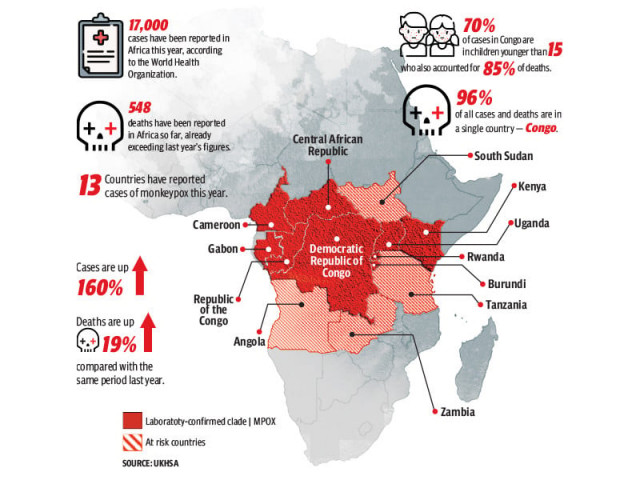
According to data from the Centers for Disease Control and Prevention in Africa, more than 17,000 mpox cases have been reported across the continent since the start of 2024, surpassing last year's total. This surge, coupled with the haunting memories of the World Health Organization's (WHO) last global alert before the Covid-19 pandemic, has raised alarm. Medical practitioners believe that death rates may vary due to factors like access to healthcare and underlying immunosuppression, including undiagnosed or advanced HIV. So far, data provided by the WHO indicates a fatality rate ranging from 0.1% to 10%.
What does the global mpox alert mean?
A public health emergency is typically declared when a disease or its variant is spreading rapidly, as is the case with mpox. Since 2022, more than 99,000 confirmed cases of the infectious disease have been recorded through July 2024. Two years ago, a similar alert was issued by the WHO, and evidence shows the outbreak was eventually controlled through behavior changes and vaccines. However, media reports indicate that mpox has been a concern in parts of Africa since 1970, with regular outbreaks. Experts at the global health body have described the recent spread as Congo's worst, resulting in over 1,100 deaths since January 2023, predominantly among children.
Now, data gathered by the WHO shows that two strains of mpox are circulating in Congo: the endemic clade I and a new variant, clade Ib. According to Reuters, clade Ib has spread from eastern Congo to Rwanda, Uganda, Burundi, and Kenya. Outside Africa, Sweden has reported the first case of this new variant, while Pakistan has yet to confirm its version of the virus. As the global community rushes to provide medical resources and funding to Congo, health experts stress the need for rigorous surveillance at both national and individual levels to prevent the disease from spreading further and escalating into a global pandemic.
How concerned should we be in Pakistan?
Pakistan's first case of mpox was confirmed on August 16, when a returning traveler from the Middle East was detected at Bacha Khan International Airport in Peshawar. It remains unclear whether the case involves the new variant or the clade that has been spreading globally since 2022.
In response, both federal and provincial governments have swiftly implemented checks at all points of entry across the country. According to details gathered by the Express Tribune, major airports are now screening all international passengers entering Pakistan.
Dr. Faisal Mahmood, Associate Professor of Infectious Diseases at Aga Khan University Hospital, noted that mpox is less contagious than recent outbreaks such as Covid-19. "Unlike the coronavirus, mpox isn't as widely spread or as contagious," he said. "When the WHO raised the threat level in 2022, Pakistan only saw a handful of cases, and we expect a similar situation this time. Most cases will likely come from returning travelers, with some potential for limited local transmission. Overall, there is little reason for the general public to be alarmed," Mahmood explained.
According to a document published by the National Institutes of Health (NIH), there have been 11 reported cases of mpox in Pakistan since 2023, with one death, as of August 15, 2024. The document, titled "Revised National Guidelines for Mpox," confirms that there is no scientific evidence of local transmission to date.
While all ports of entry are on high alert, Mahmood was also asked about Pakistan's healthcare infrastructure and its capacity to manage mpox should the virus spread. "Overall, we should be okay." Mpox, he explained, requires relatively close contact to spread, and patients do not need special air handling in hospitals. "This means many hospitals can manage these cases. Personal Protective Equipment (PPE) is also easy to obtain and not extensive for this infection." However, Mahmood cautioned, "What we lack are medications and vaccines for prevention, and those are also in short supply globally."
Asked whether temperature screenings for returning international passengers are adequate for detecting mpox, Mahmood replied, "No, because the fever associated with mpox usually lasts only one to three days before skin lesions appear, temperature screenings are not the most effective method. Visual inspection is generally sufficient for initial detection. For further verification, a polymerase chain reaction (PCR) test is necessary." Mahmood explained that this specific PCR test must be conducted by trained staff, as it involves testing the lesion itself, which needs to be unroofed. "Typically, this is done in hospitals or specialized laboratories," he added.
Is Pakistan on the right track?
In the Global South, health infrastructure is often viewed as weak due to limited resources. During the last health emergency, the Covid-19 pandemic, some governments were slow to respond or failed to implement effective measures. In neighboring India, often used as a benchmark for assessing Pakistan's efforts, more than 1.2 million deaths were recorded. At one point, funeral pyres were burning around the clock and cremation grounds ran out of space due to India's unprepared medical infrastructure, which collapsed under the strain as authorities hesitated on how to manage the crisis.
In contrast, Pakistan reported over 30,000 coronavirus-related deaths. With the trauma of the pandemic still fresh in the national memory, there is heightened concern about health infrastructure following the WHO's recent mpox alert.
Commenting on the measures taken by authorities in Pakistan, Dr. Faisal Mahmood said: "It's important to consider the current phase of disease spread and focus on preparation. At this stage, ensuring that all preparatory measures are in place is crucial. We are on the right track with screening at ports of entry, having protocols for managing mpox patients in designated hospitals, and identifying care providers." The challenge, Mahmood said, is balancing resource allocation "Deploying too many resources too early or not enough," he explained
"Currently, public health authorities are taking appropriate steps. However, improving surveillance could be beneficial, as symptoms may develop weeks after virus exposure."
"It would also be helpful to raise awareness in private sector hospitals about recognizing mpox and implementing proper reporting and isolation protocols," he added.
What are the symptoms?
According to the WHO, mpox presents a range of symptoms. Common signs include a rash lasting 2 to 4 weeks, often accompanied by fever, headache, muscle aches, back pain, and swollen lymph nodes. The rash can appear as blisters or sores on the face, palms, soles, and groin, and may also affect the mouth, throat, or genital regions. Symptoms typically resolve with supportive care, but severe cases, the global health body said, can lead to complications such as secondary bacterial infections, encephalitis, myocarditis, pneumonia, and eye issues. Higher-risk groups, including newborns, children, pregnant individuals, and those with immune deficiencies, may face more severe outcomes and require hospitalization and antiviral treatment.
How does it spread?
Medical data suggests that mpox virus spreads primarily through close contact with an infected person, including skin-to-skin contact, mouth-to-mouth contact, or being face-to-face (which can generate infectious respiratory particles). In 2022, during the global outbreak, sexual contact was the primary mode of transmission. Scientific research related to the disease shows that the virus can also persist on surfaces such as clothing, bedding, towels, and electronics touched by an infected person. Patients who have tested positive with mpox are considered infectious until all lesions have crusted over, scabs have fallen off, and a new layer of skin has formed, typically taking 2 to 4 weeks. The virus can affect various body parts, including the mouth, throat, and genital regions.
What treatment options are available?
While medical understanding of mpox is growing, the World Health Organization acknowledges that it remains limited. Two years ago, the global health body's $34 million appeal to combat mpox failed to attract donor support, and vaccine access remained highly inequitable. African countries, in particular, lacked access to the two vaccines used during the global outbreak. The situation has seen little improvement, though efforts to address it are ongoing, with the WHO recently appealing for vaccine donations from countries with stockpiles.
Commenting on treatment options, Dr. Faisal Mahmood of Aga Khan University Hospital said: "There are about three vaccines available for mpox. But mass vaccination isn't generally recommended since mpox is typically spread through close contact."
He added that those at high risk, such as individuals in contact with mpox or those with risk-enhancing behaviors, should be vaccinated. However, he noted that vaccines are currently unavailable in Pakistan, as is the case in much of the world.
"For most mpox cases, supportive therapymeaning symptom managementis usually sufficient. The lesions can be quite painful, so managing pain and preventing secondary infections is key," Mahmood explained. "There is one medication currently under trial, but unfortunately, these trials aren't taking place in Pakistan. However, in most cases, supportive care and symptom management should be enough," he added.
Asked about high risk individuals, Mahmood said: "Generally, as with other infections, individuals with low immunity are more likely to experience severe outcomes from mpox. This includes patients with advanced HIV or those undergoing chemotherapy. People with weakened immune systems struggle more to control the virus, which can lead to worse outcomes."
The other dangers
Since the confirmation of Pakistan's first mpox case, social media accounts on X (formerly Twitter) have contributed to the swirl of misinformation, with some Indian-based accounts spreading unfounded claims about the number of confirmed cases in the country. The Hindu, a prominent English-language newspaper in India, citing Reuters, reported three confirmed cases of mpox in Pakistan, while local authorities have confirmed only one case to date. Similarly, News18, formerly affiliated with CNN and now owned by Reliance Industries Limiteda group with ties to the Bharatiya Janata Party (BJP)reported the same figure.
Dr. Faisal Mahmood highlighted misinformation as a major concern. "Social media and heightened alert levels have created unnecessary fear that mpox will spread rapidly, which is unlikely since it is not highly transmissible." He also noted confusion between mpox and chickenpox due to overlapping symptoms. "Chickenpox is much more common and more easily transmitted. Overall, the most important message is to stay calm as we are unlikely to be significantly impacted by this virus," he added.
Does the virus have the potential to spread?
The WHO's designation of mpox as a "public health emergency of international concern" last week has put the world on notice. The virus has already caused a significant number of deaths in parts of Africa, particularly in the Republic of Congo. The main concern for many countries, including those with confirmed cases outside Africa, is how extensively the virus might spread. When a similar alert was issued two years ago, the outbreakthen known as monkeypoxaffected nearly 100,000 people worldwide, including over 32,000 in the United States. Triggered by mpox's recent spread to a dozen additional African countries, the current alert, health experts believe, is still manageable. However, they warn that its future impact hinges on the global response to managing what could become a more severe health crisis.
Dr. Faisal Mahmood of Aga Khan University Hospital observed, "We might see a pattern similar to earlier mpox surges, where the virus spread primarily within close contact networks such as social or sexual groups." In the context of Pakistan, he added, "If mpox were to enter similar networks here, it could potentially spread more widely within those groups. This is why the situation is being monitored closely." (With additional INPUT by Tufail Ahmed, Wisal Yousafzai, and Muhammad Ilyas)



















COMMENTS
Comments are moderated and generally will be posted if they are on-topic and not abusive.
For more information, please see our Comments FAQ