Healthcare at your fingertips
Covid-19 has accelerated a global push towards digital delivery of essential services, especially in telemedicine
KARACHI:Many countries have seen a boom in digital transformation following the pandemic. One of the areas that saw this transformation was telemedicine healthcare - medical services delivered through digital and other means. The main reason was to continue to provide healthcare remotely and safely during the pandemic. However, experts worldwide now believe that although Covid-19 may have given a rise to telemedicine, this practice may be here to stay.
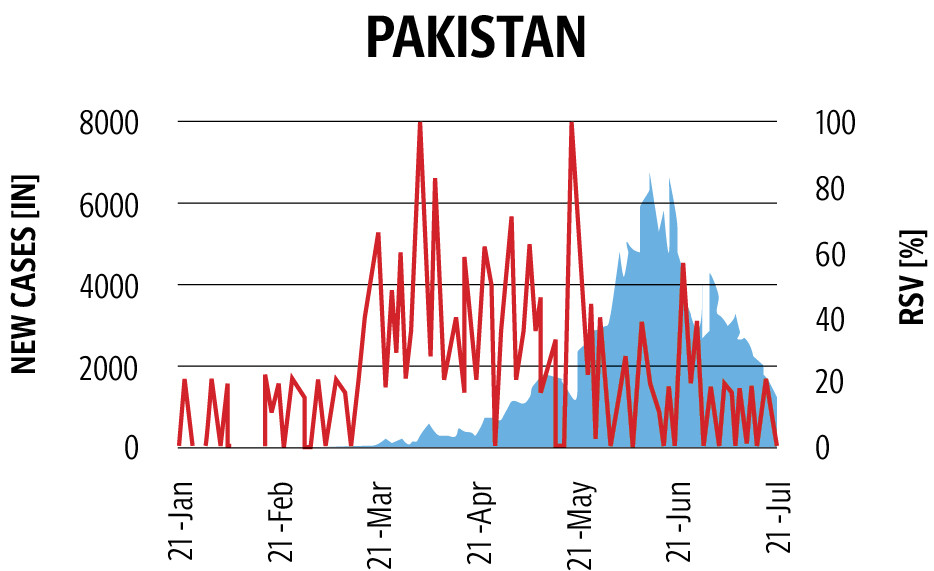
The type of healthcare system that was available even before the Covid-19 pandemic proved to be important in the lockdown situation and in the context of stretched or unavailable health systems. In Pakistan, more than 928,588 Covid-19 cases were recorded by June 2021, resulting in 21,105 deaths in total after the second wave, which was more deadly than the first. Since January 2021, Pakistan has seen an increased surge in daily cases to over 6,000 in mid-April, causing a dire situation in the hospitals due to a lack of resources and an increasing number of issues.
Since March 2020, the country saw multiple lockdowns that inhibited many patients from getting timely treatment for Covid-19 and other related issues in a healthcare system that is already fractured. Although the lockdown was lifted multiple times, many hospitals struggled to cope with the increased demand for qualified healthcare experts to deal with the ongoing pandemic.
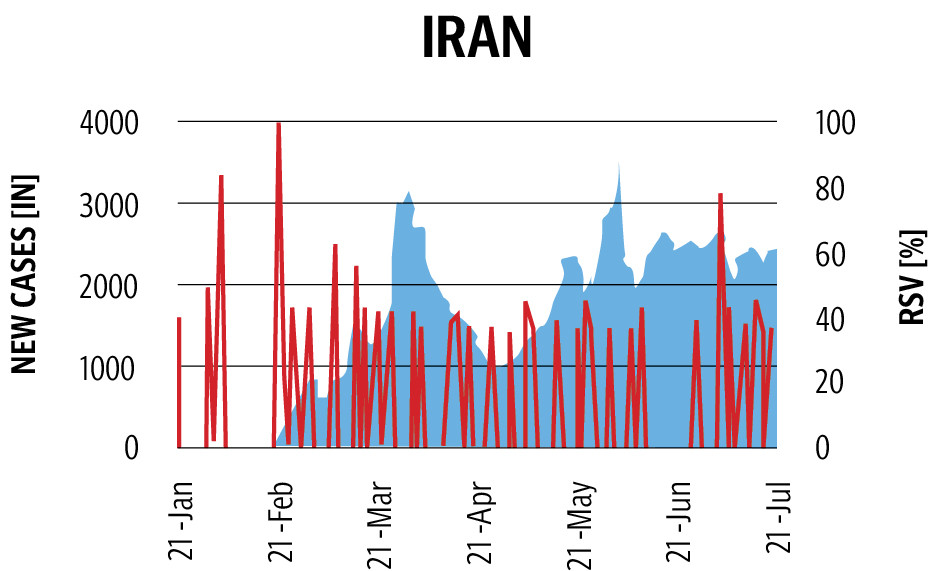
Not only Pakistan but many countries worldwide faced issues in catering for the increasing numbers of not just Covid-19 patients but also patients struggling from other conditions. Patients across the world were also feared visiting hospitals to in order to avoid Covid-19 exposure. Infants, kids, pregnant women, the elderly and patients with pre-existing health conditions are at higher risk of getting Covid-19 while also needing medical help. Telemedicine, during this time of the ongoing pandemic, played a pivotal role in acting as a bridge for of those vulnerable patients who needed treatment.
A team of healthcare experts globally discussed the rising issue at the Fifth edition of Abbott's Annual Growth Summit, a conference that focuses on finding solutions to end childhood malnutrition globally. The critical point in this year's edition was how the healthcare centres experienced a shift to online, and technology-enabled care services (TECS) gained a boom.
Executive Vice President of Nutritional Products Abbott Daniel Salvadori said, “Childhood malnutrition is a worldwide challenge, and we are committed to finding a solution to it together so that every child live the same life.”
According to Clinical Academic Pediatric Dietitian Dr Luise Marino, Covid-19 significantly impacted the access to healthcare, nutritional status and food security of millions of children worldwide.
“Almost overnight, routine nutrition and healthcare appointments were offered virtually via telehealth and TECS. Almost 12 months on, we explored the experience of paediatrics dietitians with regards to TECS. Our survey suggests the majority of paediatric dietitians found TECS as overwhelmingly positive,” she said during a session on Navigating Remote Care for Paediatric Nutrition Management at the AGS 2021.
“Facilitators for a positive experience were lower rates of non-attendance, ability to have insight into the home, time efficiencies for both paediatric dietitians and parents. In addition, reduced risk of Covid-19 infection and more time for dietitians to complete dietetic notes was reported,” she added.

Creative: Mohsin Alam
Telemedicine boost in Pakistan
During this time, many organisations who were already working on telemedicine experienced a boost in the use since the Covid-19 began. Before that, the adoption in the urban areas was relatively low. A telemedicine service in Pakistan, doctHERs, who use technology to promote health awareness, conduct medical screenings, deliver consultations and provide access to prescription medicines for low-income, high-risk and underserved communities while building local frontline health workers, saw the adoption of the service in urban areas too.
"Pre pandemic, patients in the rural areas were our focus who were not able to get the basic healthcare services. They were able to get in contact with the qualified doctors on audio and video call. The adoption of telemedicine in the urban population was quite low as they preferred going to the doctor in-person rather than on-call," said doctHERs CEO Khaqan Sikander to The Express Tribune.
According to Sikander, there was approximately a 25 to 30 per cent increase in telemedicine in urban areas since the lockdowns. “People in the urban part of the country were not as much adoptive of the service as in-person check-up facilities were available but now since the lockdowns, they have no option but to adopt telemedicine. This has given a significant boost to the recognition of the service, which will now stay [after the lockdown and pandemic]," he said.
Like doctHERs, services like Aman TeleHealth, a 24-hour healthcare helpline that provides easy and timely access to diagnostic services, primary medical advice, mental health and family planning counselling over the phone also increased. Aman TeleHealth has over 10,000 healthcare facilities mapped out on its system, enabling callers to access information about the relevant facilities in their vicinity.
Analysing the situation in Pakistan, the United Nations Development Programme (UNDP) Pakistan partnered with Sehat Kahani, a healthtech social enterprise with a network of 27 e-clinics across Pakistan that connects patients to qualified doctors via a telemedicine based mobile and web solution— to accelerate the efforts to support Pakistan's healthcare system. Physicians and specialists of Pakistani origins were reached out through 'Yaran-e-watan' to continue their practice through the telemedicine platform.
The mobile application was made free for accessing teleconsultations for the patients to avail health services through their smartphones within the vicinity of their homes. A 24/7 helpline was also launched to provide Covid-19-related information, referral to an online doctor for suspected cases and follow-ups during home isolation for positive patients. According to Sehat Kahani, more than 300,000 consultations have been done, out of which 3 per cent were Covid-19 suspects.
To further accelerate telemedicine, UNDP and Sehat Kahani also collaborated with the Ministry of National Health Services, Regulation and Coordination (MOH) in upgrading 60 ICUs in Pakistan's public and private hospitals to tele-ICU using the application. This helped the ICU's staff to connect to teams of skilled critical care nurses and intensivist doctors to monitor thousands of patients at hundreds of hospitals virtually. This remote monitoring technology at the ICUs provides an added level of clinical support and helps hospitals prevent potential patient complications.
UNDP Pakistan Project Manager of Youth Empowerment Programme Laura Sheridan, describing the multipronged advantages of telemedicine platform said, “Telemedicine can be an accessible and affordable route to providing quality healthcare to patients, especially those in remote communities where healthcare systems are inadequate. It also maximises the potential of women physicians who are not being utilised to their full potential owing to societal and cultural norms.”
Enabling a healthcare revolution
Although telehealth services are now available in many countries worldwide, private and public health providers are facing issues in implementing and scaling up these services systematically and cost-effectively.
Luise believes that as this healthcare revolution is set to stay, healthcare professionals and parents should continue to expect quality services irrespective of how this may be delivered. “As part of TECS consultations, healthcare professionals need to consider aspects around parental access to WiFi and software required for consultations,” she said.
Applications such as doctHERs, Marham, OlaDoc, Sehat Kahani, are providing the platform to get in contact with qualified doctors but in a country like Pakistan, many of the rural areas or even people living in urban areas don't have access to the internet or don't have the required equipment to use it.
The challenges typically relate to low client and provider adoption rates, weak health workforce capacity and digital infrastructure (and digital exclusion), and issues relating to service quality, data privacy and institutional resistance to digital disruption. In addition, the rapidly evolving technology space and the overwhelming diversity of available tools have made it difficult for actors in health systems to identify, adapt or develop solutions that are appropriate to their specific context and needs.
A doctor at the government hospital in Karachi, Sadia Manzoor, who has also adopted telemedicine, said that this is the future. “The world has evolved during the pandemic, and we all got to know the positive side of telehealth. It was present before but the way it has evolved worldwide, the patients have started to accept this as the convenient way of consulting a doctor,” she said, adding that there is still some issue regarding the connectivity and availability of equipment, but all are solvable problems.
“We also encourage the patients to go for telehealth as it is quick, convenient and safe, especially for the children during the ongoing pandemic,” she said. “The problem arises when we see that despite all the digital boom, there are still many people who don't have access to internet connectivity and don't have the necessary arrangements to opt for telehealth.”
However, she said that the people who are adopting telehealth are happy, as they don't have to spend time in waiting areas at the hospitals and can access quick consultations from home.
Talking about the future of telehealth globally, Luise believed that future research needs to consider some of the factors to improve telehealth. “They need to consider how to develop and implement strategies for parents to complete accurate anthropometric measures within the home, and finding innovative ways to build a rapport with parents as well as assessing non-verbal cues as part of virtual consultations,” she added.
Here to stay
On the other hand, Sikander believes that although telemedicine has seen a significant increase, it is temporary. “Right now, people are adopting because they don't have any option. Most of the people in Pakistan or any other country still prefer in-person check-ups. The reason that people are adopting telemedicine is that they are not able to go in-person,” he said.
“As we are getting vaccinated and things are going towards normalisation, we will again see a decrease in the number of patients using telemedicine. Our work has increased almost by 100 per cent but that is temporary. Still, if we look at the overall number, yes there will be an increase as compared to the pre-covid situation,” he said.
Talking about keeping people to stick to telemedicine, he said that the patients cannot be forced to use any service. They should be given an option. “If we only focus and promote telemedicine, this will not attract them. We have to offer both options, telemedicine and in-person check-up. The combination of both will enable them to use telemedicine,” he said.
He also pointed out that the people in Pakistan use healthcare services reactively. They have to use it proactively. “We wait for the disease to develop, whereas we should stop it before being developed. This is the type of approach we have in Pakistan which needs to be changed and telemedicine can help in real-time,” he concluded.

COMMENTS
Comments are moderated and generally will be posted if they are on-topic and not abusive.
For more information, please see our Comments FAQ