“Is there good news?” In a culture where newly married couples are constantly bombarded by prying friends and family over their plans for a baby, pregnancy is generally seen as a beautiful blessing paving the way for a new life to enter the world. Yet, what precedes the arrival of the bawling bundle of joy is a ninth-month long period of precarious waiting, which can often meet an unfortunate end, whether by fate or by choice.
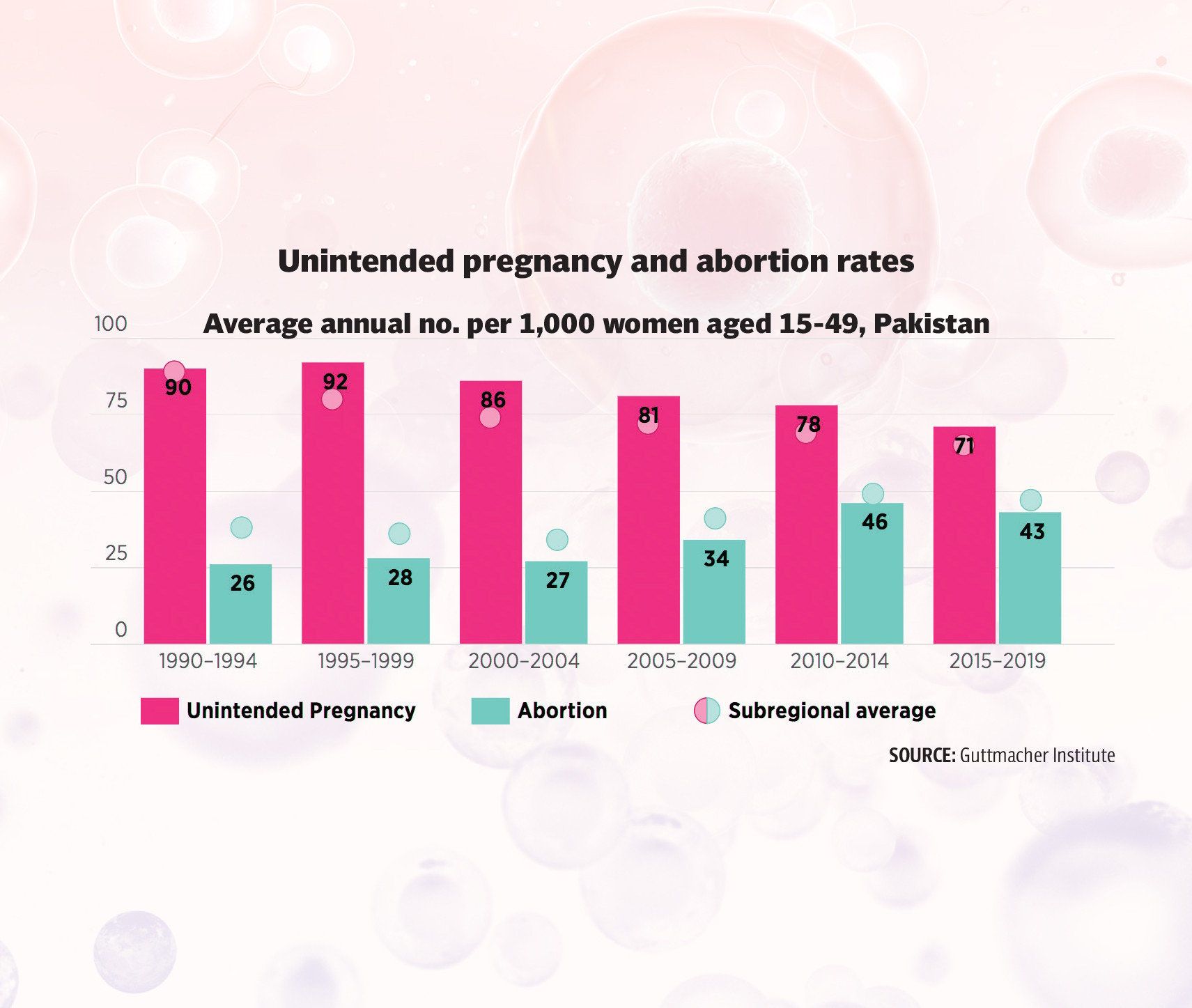
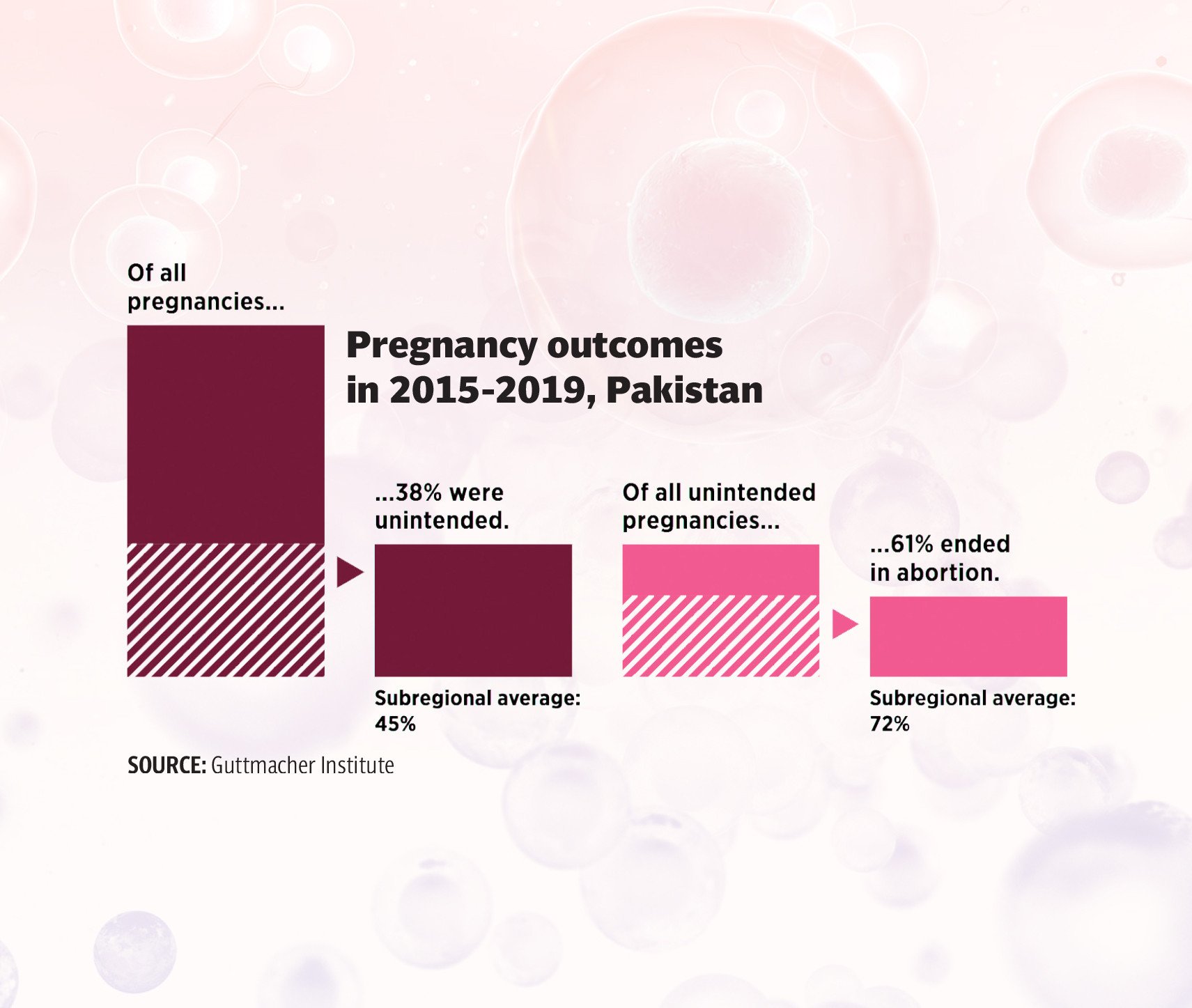
As per data obtained by the Pakistan Demographic Health Survey Report (PDHS) for 2023, an estimated 870,185 women across Pakistan required treatment for post-abortion complications resulting from either spontaneous or induced abortion, with the highest, 52 per cent of all cases reported in Punjab.
When the correspondents reached out to public hospitals across the country, none were willing to share any data on the number of women seeking treatment for post-abortion complications. “Since induced abortion is a taboo subject and is not allowed by the law, hospitals would be hesitant to share data even on miscarriages. However, I can tell that the number is pretty high. Although women’s reproductive health is not a stigma, it’s not a high priority either,” opined Dr Yasmeen Sabeeh Qazi, former senior country advisor on family planning and maternal, neonatal and child health to the Bill and Melinda Gates Foundation.
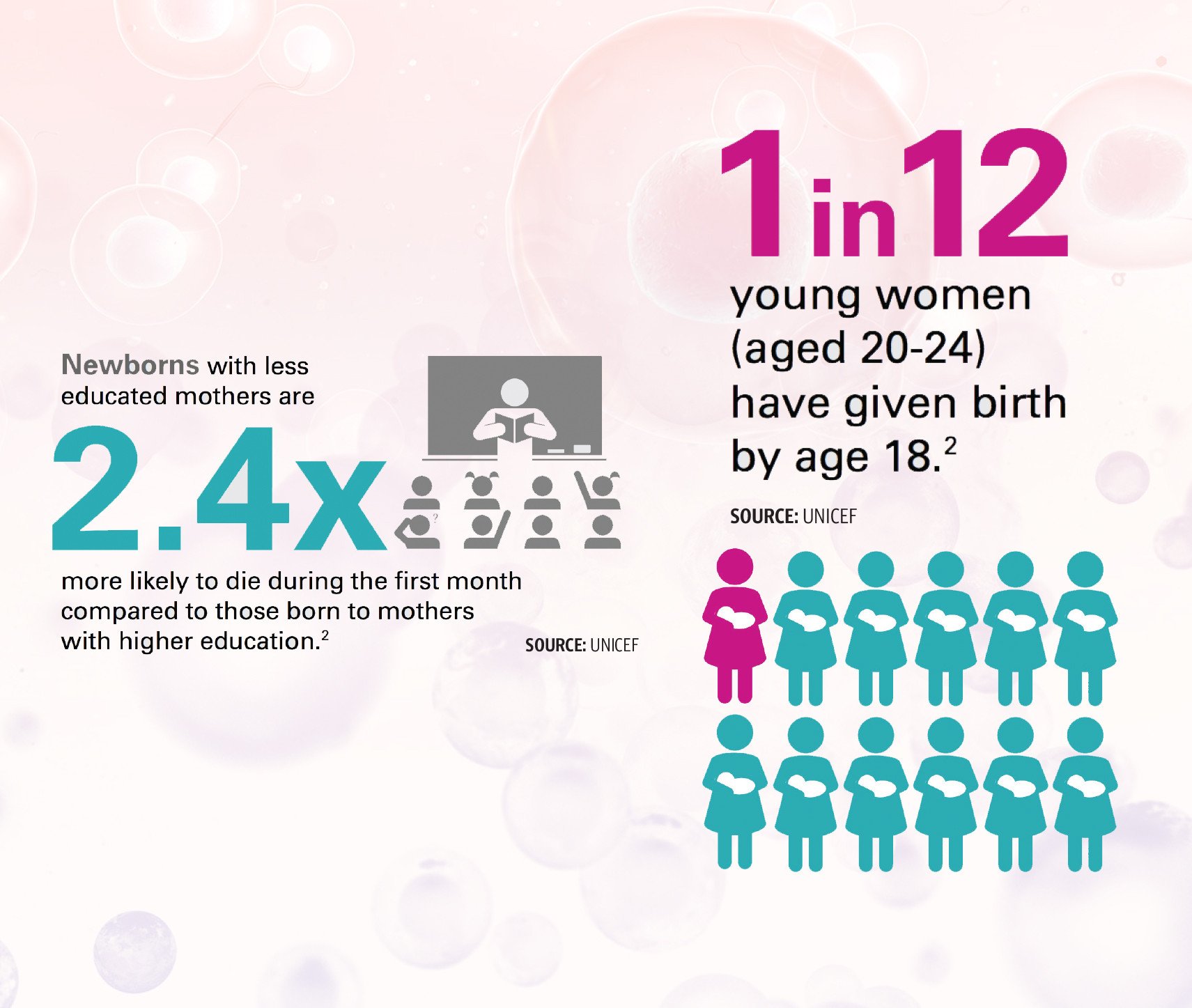
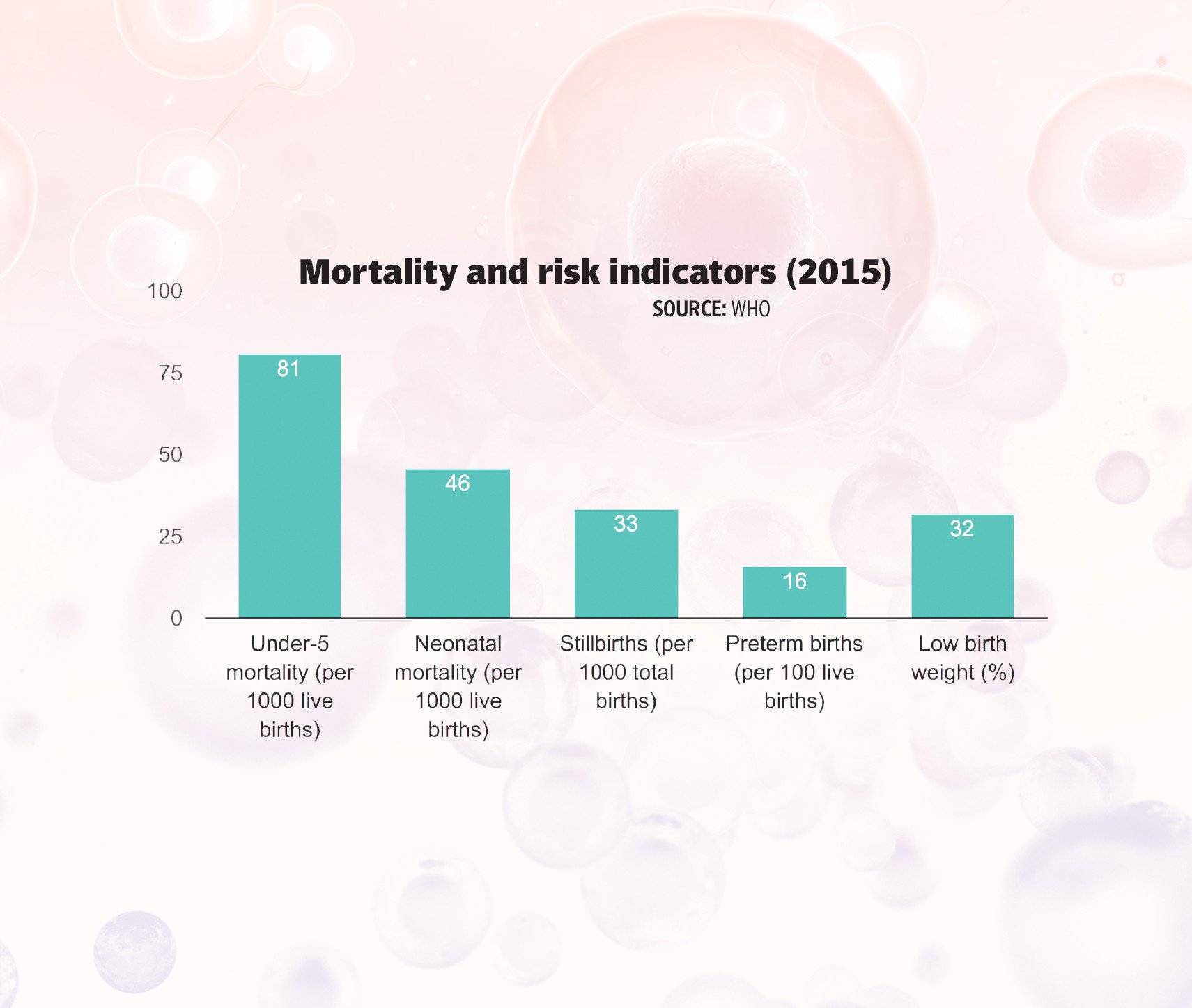
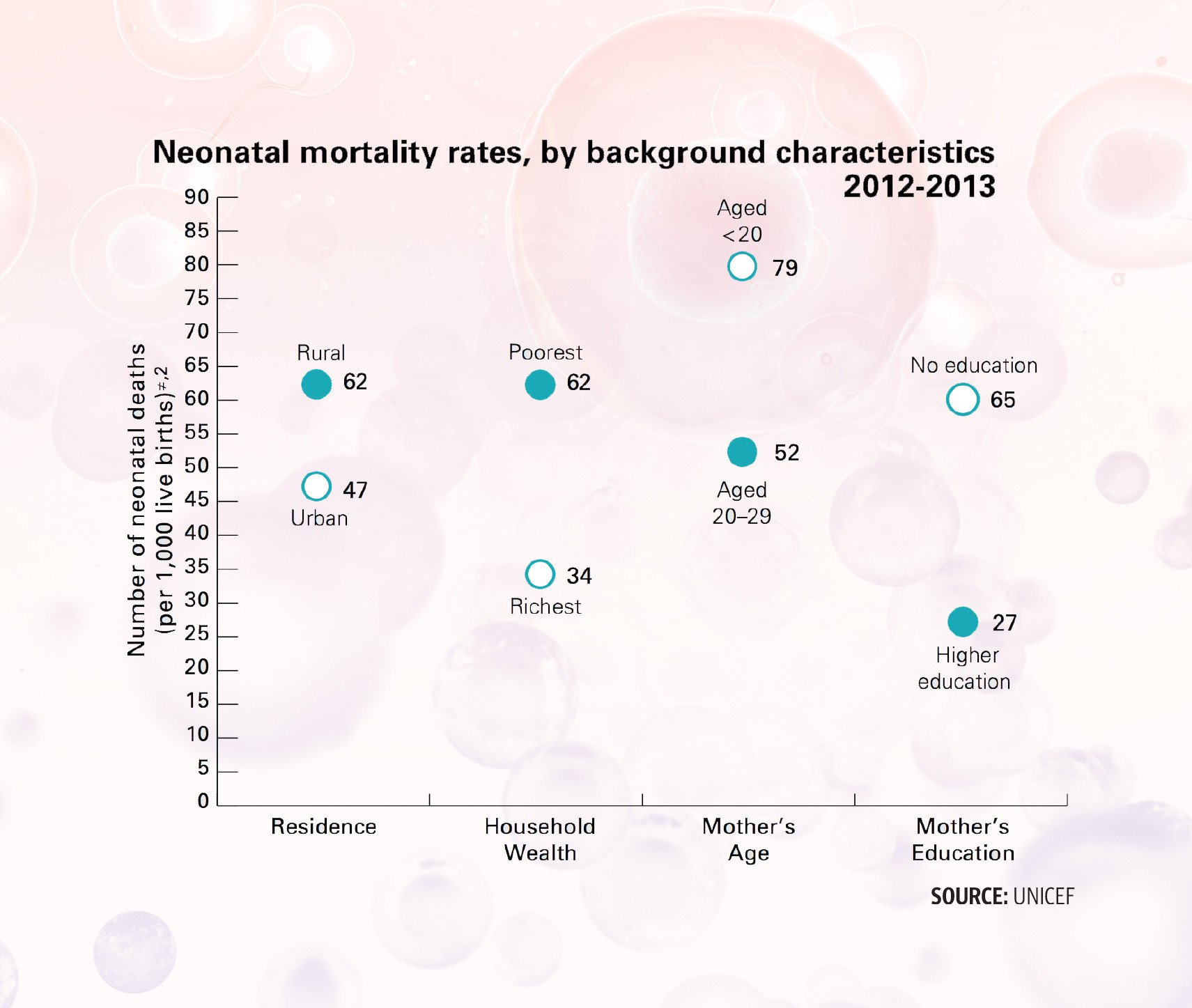
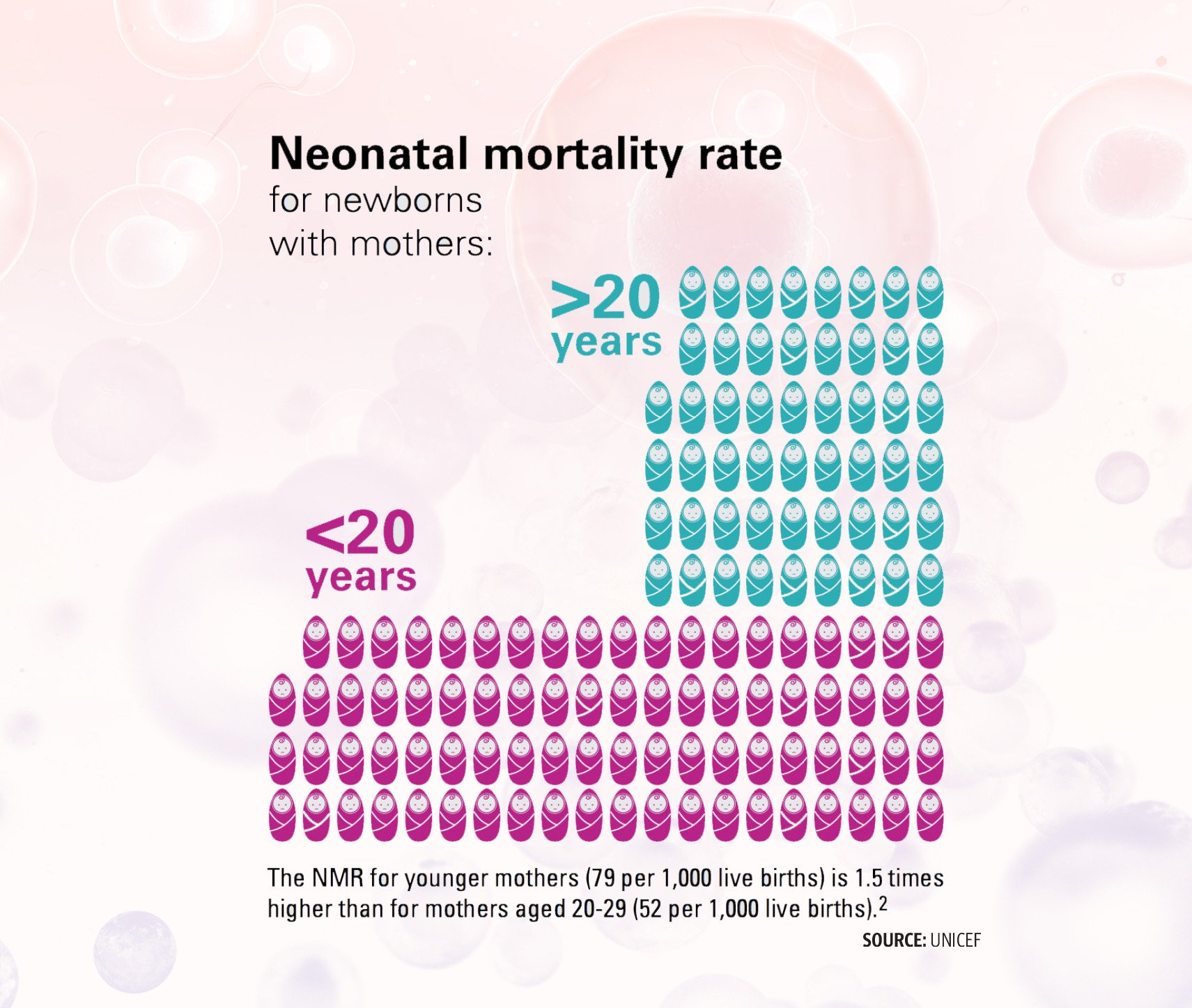
According to Dr Tayyiba Wasim, Head of Gynaecology at the Services Hospital, nearly 15 per cent of all pregnancies end in a miscarriage. “The miscarriage ratio is high among women with a history of nutritional deficiencies, low bodyweight, restricted eating, genetic disorders and lack of medical counselling. Hence, those married off at an early age are also at an added risk,” she said.
The issues highlighted by Dr Wasim are just the tip of the iceberg in Pakistan, where misogynistic blame, son preference, domestic violence, hazardous working conditions, chronic stress, substance use, unsafe abortions and outdated post-abortion treatment's silently plague the physical and mental health of the country's reproductive-aged female population.
Outdated post-abortion treatment and medical arrogance
Imagine rushing to a hospital emergency with an injured hand only to be told by the doctor that they will be burning the open wound with a hot rod to stop the bleeding. Traumatised, right? In today’s time and age, nearly every person would be, since cauterisation is no longer used for treating cuts and abrasions after the invention of sutures.
While the following scenario may be hypothetical, doctors’ refusal to shift to modern methods out of sheer medical arrogance is a painful reality for women seeking treatment for post-miscarriage or abortion complications at hospitals across Pakistan, which continue to use the outdated method, dilation and (sharp) curettage (D&C) despite the World Health Organisation (WHO) discouraging the procedure for pregnancy loss before 14 weeks of gestation.
Shazia, a 22-year-old hailing from Tando Muhammad Khan, bled throughout her pregnancy, which ended before 12 weeks of gestation. After being examined at the Civil Hospital in Karachi, she was told that blood clots in her uterus had not fully evacuated hence she required a D&C. “After the procedure, my wife had to stay in the hospital for three days since she required blood transfusions,” recalled Shazia’s husband, who regretted the unavailability of modern gynaecological facilities at hospitals across the province.
Like Shazia, the wife of Chandio, was also given a D&C at the Jinnah Hospital after she suffered a miscarriage, even though she was only 4 weeks pregnant. “My wife fell from the stairs, due to which she suffered severe bleeding. After the ultrasound, the lady doctor took our permission for D&C. Once the procedure was done, my wife was transferred to the ward,” said Chandio.
Dr Malahat Mansoor, Head of Obstetrics and Gynaecology at Sahara Medical College Narowal confirmed that D&C was not recommended at all for treating post-miscarriage complications since it required general anesthesia and could result in significant post-surgical complications. “D&C inflicts significant trauma to the patient,” said Dr Mansoor.
According to the WHO, since dilatation and (sharp) curettage (D&C) before 14 weeks of gestation causes significant pain and suffering to women, it is a major human rights violation and is not recommended. Similarly, Pakistan’s Ministry of National Health Services Regulations and Coordination (MoNHSRC) has also recommended against the method due to its high risk of complications including infection, excessive bleeding, uterine tearing, cervical laceration and haemorrhage.
Unfortunately, in spite of the global and local health recommendations, data obtained from the Guttmacher Institute revealed that 50 per cent of 596 public and private facilities across all four provinces were still performing D&C for treating post-abortion complications while manual vacuum aspiration (MVA), the WHO recommended, modern method, was only used in 24 per cent of healthcare facilities.
“D&C has been the traditional method of evacuating the uterus in the case of miscarriage and abortion. Since D&C is essentially a curettage, which involves hurting the lining of the uterus, it could be painful for the woman and also lead to complications in case the provider is not trained. It was completely discouraged by the WHO ten years ago and has been replaced by MVA, where the contents of the uterus are aspirated instead of hurting the lining. Back in 2011 and 2012, when the movement to shift to MVA had started after the WHO guidelines were issued, we started asking all the providers in Pakistan to not to use D&C and to shift to MVA,” claimed Dr Qazi.
Dr Qazi opined that if a large percentage of providers were still using D&C, it was primarily a matter of mindsets. “It takes a lot of time for providers to shift from something that they are comfortable with. The comfort of the patient is not a priority. Since the doctors have an elevated confidence in their expertise, they feel they can do no harm. This attitude withholds them from understanding that MVA is a safer and much better technology causing much less pain to the patient,” observed Dr Qazi.
“Apart from this, another reason behind the partial shift to MVA in the private sector, is the cost and availability of the equipment. Since there is very little demand for MVA, its availability is not guaranteed. Therefore, initially even those provided who had converted to MVA could not find a consistent supply of the paraphernalia, therefore they resorted back to D&C.
“When it comes to the public sector, we were able to include MVA in the national drug list but due to supply and demand issues, the shift couldn’t happen completely. Furthermore, doctors were also not trained on its usage. It’s not rocket science, but it still requires training,” commented Dr Qazi, a public health expert.
Pregnancy loss, misogynistic blame and mental health
Nadia Khan, a 25-year-old patient from Charsadda spotted at a hospital in Peshawar, shared her heartbreaking encounter with her husband and in-laws after she miscarried her third child.
“My husband has been convinced to divorce me since he believes the baby died due to my negligence. I already have two daughters, and the family was eager to welcome a baby boy. However, all my hopes have been shattered,” cried Khan, who apart from undergoing the physical pain of miscarriage was also subjected to mental and emotional torture by her heartless husband and his family.
According to Dr Uzma Ashiq Khan, Clinical Psychologist and Assistant Professor of Gender Studies at the Lahore College for Women University (LCWU), a woman’s ability to deal with a miscarriage depends largely on her socioeconomic class, family structure and her support system.
“Societal pressure surrounding miscarriages leads to stress in women. Therefore, the support of the family is crucial to help women deal with pregnancy loss and prevent further miscarriages. These attitudes are worse for women who have no child or those who have daughters and are unable deliver a son,” she opined.
“Postpartum depression, which can also occur after a miscarriage is still an unknown concept among the large majority of our population. Even though men also face societal pressure in the aftermath of recurrent miscarriages, the burden of reproduction lies on women. Even in cases of infertility, families refrain from getting the male partner tested, even though the male infertility tests are less expensive and can offer a quick diagnosis. The focus on the female partner in fertility issues delays treatment and worsens complications,” she said.
Medical research supports Dr Uzma’s speculation. A report published by the European Society of Human Reproduction and Embryology revealed that the health of fathers-to-be was associated with more than a quarter of pregnancy outcomes, which might end in a miscarriage if the father had obesity, diabetes, high blood pressure or high cholesterol levels. Similarly, a study by the Wiley Online Library also showed that the risk of miscarriage before 13 weeks was 74 per cent higher when the father’s age exceeded 45 years.
Dr Uzma opined that the primary issue was that such conversations were non-existent in our society. “Right from the moment of puberty, issues concerning women’s bodies are hushed therefore, there is a general lack of awareness on the unique social causes of miscarriages,” she highlighted.
Malnutrition, early marriages, and unplanned pregnancies
“Girl’s should eat less, no one wants a chubby bride.” “Marry your daughter off at an early age, otherwise she won’t adjust with her husband.” “Children are a blessing from God, why plan them?” For a society where even educated families nurture such ridiculous beliefs, perhaps it is no surprise that malnutrition, early marriages and unplanned pregnancies have emerged as the primary reasons behind women’s poor pregnancy outcomes.
According to Dr Qazi, malnutrition and stunting is a major challenge plaguing Pakistan and is indicative of a national emergency as serious as polio and Covid-19, which needs to be addressed immediately. “More than 50 per cent of children are malnourished because the mother suffered from some nutritional deficiency before pregnancy,” said Dr Qazi.
“Since there is no concept of preconception counselling or family planning in the country, young girls get pregnant with untreated iron, folic acid or vitamin D deficiencies, which increases the risk of miscarriage,” added Dr Hasan.
Therefore, Dr Qazi believed that nutrition counselling should start before or around the time girls started menstruating. “Today, the situation might be better but when I started my career, gender-based discrimination in nutrition was a common problem. Sons were given meat while daughters would eat from whatever was left. The belief that boys required more nutrition compromised girls’ health. Hence, we see that more than 60 to 70 per cent of girls develop iron-deficiency anaemia once they start their menstrual cycle,” noted Dr Qazi, who revealed that the risk of miscarriage was further magnified by early marriages.
According to the PDHS 2017-18, the mean age of marriage for women in Pakistan is between 19.4 and 20.0 years while the average age at first pregnancy is 22.8 years, which is five to six years less than the mean age in developed countries like the US, where most women have their first child by the age of 27 years, and the UK, where the first childbirth usually occurs at the age of 29 years.
A 2019 study conducted by the BMJ, a leading medical research journal, concluded that the risk of miscarriage was lowest, around 10 per cent, when women conceived a child between the ages of 25-29. Hence, it is evident that most Pakistani women are conceiving children outside the optimum time frame safest for the mother and child.
“In order to improve women’s preconception health in Pakistan, parents and husbands need to take a proactive role. They must ensure that women’s nutritional needs are met through supplementation and counselling before pregnancy,” highlighted Dr Qazi.
Domestic violence and medical apathy
For the typical macho husband accustomed to reaching for his shoe at the slightest offence, the vicious cycle of domestic violence rarely ceases when his nagging wife happens to be carrying his own flesh and blood.
According to the Human Rights Commission of Pakistan (HRCP), a whopping 90 per cent of women have suffered some form of domestic violence in their lifetime while approximately 28 per cent of reproductive-aged women between 15-49 years have experienced physical violence at the hands of their husbands.
“Undocumented and documented cases show that domestic violence during pregnancy is pretty common and has a very strong impact since any kind of violence, particularly during the first trimester, can lead to miscarriage,” informed Dr Qazi.
Dr Saima Khan, a Peshawar-based gynaecologist confirmed that domestic violence was often an unspoken cause behind miscarriages among women in her vicinity. “Clashes with the husband or his family can quickly take a violent turn, and the battered woman loses her baby,” revealed Dr Khan.
Although Dr Khan was keen enough to decipher the concealed suffering of her patients, such trauma sensitivity is absent among the majority of providers in the country, who are not trained to identify and report signs of abuse among pregnant women.
In countries like the US, intimate partner violence screening is a mandatory study component for all third-year medical students as part of their core obstetrics and gynaecology clerkship. Therefore, all general practitioners are qualified to covertly counsel domestic violence victims, who might otherwise not have the courage to escape an abusive relationship.
“One of the solutions to address violence among women especially during pregnancy is to sensitise and train the providers including doctors and mid-level providers like lady health workers (LHW) either during their medical education or on the job. Since the LHW’s are from the community, they are aware when domestic violence is happening. Hence, they should know how to counsel a victim and help her protect herself and her baby,” urged Dr Qazi.
Hazardous workplaces, smoking and chronic stress
While elite pregnant women can afford to complain about swollen feet and morning sickness, for the hapless working-class women employed in high emission industrial zones, the next meal for the family depends on them trudging tirelessly in an insufferable atmosphere.
"Women working in environments with smoke and high emissions are at a higher risk of miscarriage. If they are provided with protective equipment, the miscarriage rate can be reduced,” said Dr Hasan.
“Families living below the poverty line, send their women to work in factories even during pregnancy. Due to the exerting nature of the job, they are unable to pay attention to their health,” observed Dr Abida Bibi, a gynaecological consultant at the Civil Hospital Karachi.
According to Dr Qazi, the labour laws in Pakistan have no special considerations for pregnant women and new mothers. “The rights of pregnant working women are neither understood nor implemented by business owners. The healthcare commission should devise SOPs for pregnant women working in industrial areas, which specify what kind of care they would need and what kind of timing or exposure adjustments were necessary. But that rarely happens since in our society pregnancy is taken so lightly. Everybody gets pregnant, everybody delivers so what’s the big deal. Shifting the mindsets is as important as shifting the law and policy,” said Dr Qazi.
Speaking of mindsets, Dr Uzma believed that one major cause of stress among pregnant women was the pressure to have a son. “While people might be happy at the birth of a daughter, they are happier at the birth of a son. The incremental happiness surrounding the birth of a son says it all,” she shrugged.
“Even though doctors tell pregnant women to stay calm during pregnancy and avoid stress, they are not machines which can switch to relax mode at the flick of a button and stay unaffected by harsh familial behaviors and difficult household circumstances,” said Dr Uzma.
In addition to household stress, Dr Khan, while speaking of the social reasons behind miscarriages in K-P revealed that chronic stress arising out of the constant threat of terrorism and militancy were also to blame for cases of pregnancy loss.
Studies too have found a significant association between living in areas of conflict and the risk of miscarriage and stillbirth, with women living in fragile zones reporting a higher incidence of early pregnancy loss.
On a separate note, Dr Bushra Rani, Executive Director at Baham, an NGO working on women's reproductive health, disclosed that women who smoked cigarettes had an eleven per cent higher risk of miscarriage than other women. Similarly, if a woman drinks alcohol and other intoxicants, she too can face a similar situation,” she warned.
Illiteracy, Internet and self-managed abortion
Looking beyond the pro-life and pro-choice debate, the availability of safe abortion drugs was nothing short of a lifesaver for women in Pakistan, who in the presence of strict abortion laws, would previously end up in the unskilled hands of some quack doctor at a makeshift abortion clinic.
“When a couple decides to terminate a pregnancy and qualified doctors are reluctant to offer help, they will still get an abortion. The only difference is that it would not be safe. In such a scenario, over-the-counter abortion drugs like misoprostol have helped women abort safely however, their dosage needs to be monitored. Women taking these drugs must be literate enough to read the leaflet correctly, follow the dosage guidelines and know when to seek medical help in case something goes wrong,” explained Dr Yasmeen.
Yet where access to self-managed abortion has improved women’s reproductive autonomy, the curse of illiteracy fueled by a blind reliance on the internet can prove deadly for women popping abortion drugs like candy. The tragic story of Bushra’s daughter is here to prove the point.
Bushra *, a domestic worker from Karachi, had tried helping her daughter get rid of an unwanted pregnancy by doing a quick Google search and asking her to buy misoprostol from a nearby pharmacy. Disregarding the need to read out the correct dosage or consult a medical professional, her daughter took a random number of pills hoping to get rid of the unborn baby her husband had refused to own. Soon after, Bushra’s daughter developed severe post-abortion complications, which led her to the intensive care unit (ICU).
Such cases are not new for Dr Mansoor, who has to routinely treat women ending up in a critical state at the hospital’s emergency after a failed abortion at home. “Contrary to earlier times when women would eat herbs for self-aborting, nowadays couples are relying heavily on medical methods of termination. Women take medicines like misoprostol after searching them online but are unable to take the correct dosage. Patients who have taken an overdose start bleeding heavily and when they reach the hospital they are in shock. On the contrary, patients who have taken an underdose are unable to abort and the pregnancy continues but with an added risk of abnormality or birth defects arising in the fetus due to the drug,” observed Dr Mansoor.
According to Articles 338 and 338(B) of the Pakistan Penal Code (PPC), abortion is a punishable offense. In 1997, the PPC added a provision to Chapter XVI, Section 335, which permitted induced abortion before the organs and limbs of the child had been formed, that is up to 20 weeks of pregnancy. Induced abortions that exceeded these conditions could be punished with imprisonment from 3-10 years.
“Although PPC Articles 338 and 338(B) declare abortion as a punishable offense, it is not a crime if it is done in good faith to save the life of the woman. However, most women have started using drugs on their own to abort pregnancies, giving rise to a host of complications. Even though the actual abortion pill, mifepristone, is not available in Pakistan, women often rely on misoprostol,” said Dr Jahan Ara.
According to Noor Mehar, President of the Pakistan Pharmacist Drug Forum, the Ministry of Health in Pakistan has approved 10 brands of misoprostol tablets, which are available at an affordable price of around Rs100. “In 2023-2024, the total sales of just one brand of misoprostol reached 16 billion. This medicine, which makes the uterus contract and push out the contents of conception, can also lead to life-threatening post-abortion complications,” warned Mehar.
While post-abortion complications can be minimised by a thoughtful consideration of the chosen method, they are inevitable in the case of an illegitimate pregnancy, where the desperation of the couple to eliminate the innocent evidence of their carnal transgression often leads them to take reckless measures.
In 2021, an 18-year-old female university student was abandoned by her boyfriend outside a hospital in Lahore, after she passed away at an illegal abortion clinic due to post-abortion complications. Although the boy initially tried to escape by pretending to be a close relative of the deceased girl, the police took him under custody soon after and the actual nature of their relationship was laid bare.
Dr Uzma, a gender expert, believed that the pitfalls arising out of the vice of premarital sex uncovered the failure of the society and the state to impart age-appropriate sex education to the youth, who were more or less unaware of the consequences of their actions.
“Turning a blind eye to the current happenings in society will not help anyone. Until or unless you educate the youth on the topic using the correct vocabulary, in line with cultural and religious principles, they will remain confused and exposed to harm. When these matters are not addressed, they manifest in society one way or the other,” concluded Dr Uzma.
(*Name has been changed to protect identity)
