One day in 2016 while scrolling through Facebook, Yumna Aftab read a story on the Humans of New York page about how stem cell transplants saved the life of someone with pediatric cancer. Out of curiosity, she saved the contact number for the service listed on the page.
A few months later, her brother Moiz – who was 16 at the time – was diagnosed with Acute Myeloid Leukemia (AML), a cancer of the blood and bone marrow. Aftab remembered the internet post about stem cell transplants and called the saved number to find out whether the treatment might work for her little brother. Research in hand, she convinced her parents it was one of the few options they had.
Aftab, who was then 18-years-old, watched her brother fight for his life in a hospital bed while her family tried to figure out what to do. After consulting with doctors in India, the US, and the UK, Aftab flew with her family to India in January 2017 to attempt the transplant, but tests found that was only a 50 percent match as a donor. The hospital refused to do the transplant, and the family was told it could only be carried out as a last resort.
“In that moment, we were blank,” Aftab told The Express Tribune. “We never saved our brother’s stem cells and now he needed them.” The family returned to Pakistan after a month in India, distraught. They searched cell banks around the world to find a donor who was a closer match, eventually locating one in Germany. Once the match was confirmed, they flew back to India for the operation in April.
The body’s natural repair kit
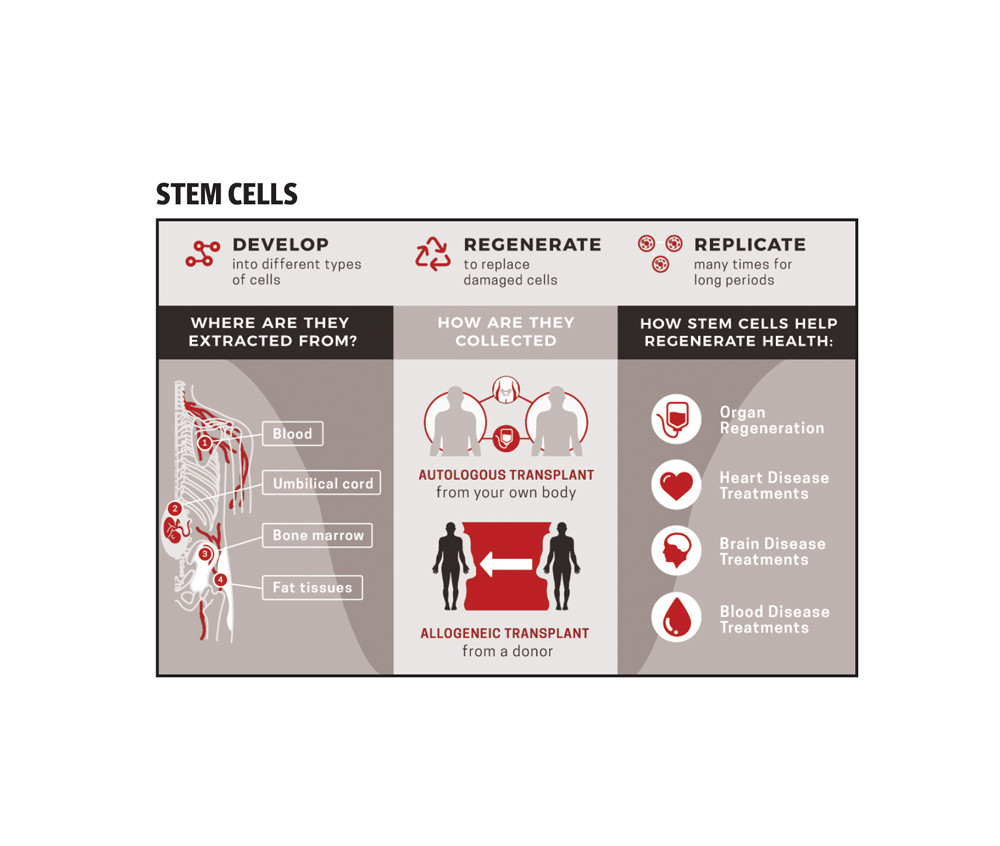
The stem cell transplant gave Aftab’s brother another chance at life and showed her family just how revolutionary the treatment can be. In addition to treating diseases like AML, stem cell transplants can be used to address an array of health conditions, including blood cancers, diabetes, thalassemia, bone marrow cancers, solid tumors, autism, as well as neurological disorders.
“It is pretty new here but still like a milestone in health sciences, its more important to save at least one can use them when needed rather than they need and they don’t have,” told Mir Mukarram Ali, regional director of Future Health Biobank in Pakistan. Future health is the largest stem cells bank in the UK and Europe and has been operating in Pakistan for the last seven years. Other than them no other bank operates in Pakistan as of now. Previously, a few US-based banks operated in the country but were unable to sustain themselves and eventually shut down. Right now other than Future Health, two other agents for international stem cell banks operate here.
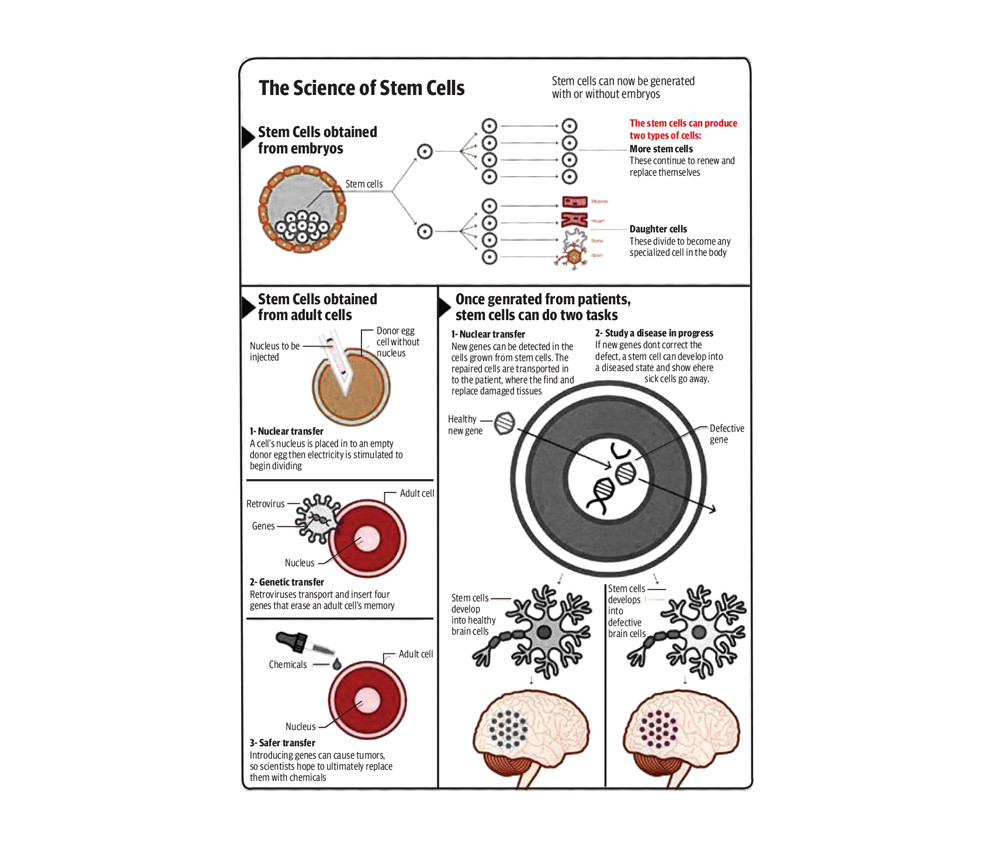
Stem cells are the repair kit of the body and can be used to regenerate cells as well. “It is like a new genetic code, which is taken at the time of birth from the cord blood and can be used for the child in future when needed to treat any deadly disease,” said Dr Ebad Baig, who has been working on stem cell technology for the last 20 years in the UK. While talking to The Express Tribune, he also said that the body constantly produces stem cells but with age, it gets immune to the diseases but the cord blood cells, which if saved at the time of birth are the genetic coding of the child and are naïve and can be used for transplant.
The matching of stem cell work through HLA typing. There are several of them and just like blood groups, they are different matches to different people but then race and geographical location are also a very important factor and with different race, the probability and acceptance of the body has a lower chance.
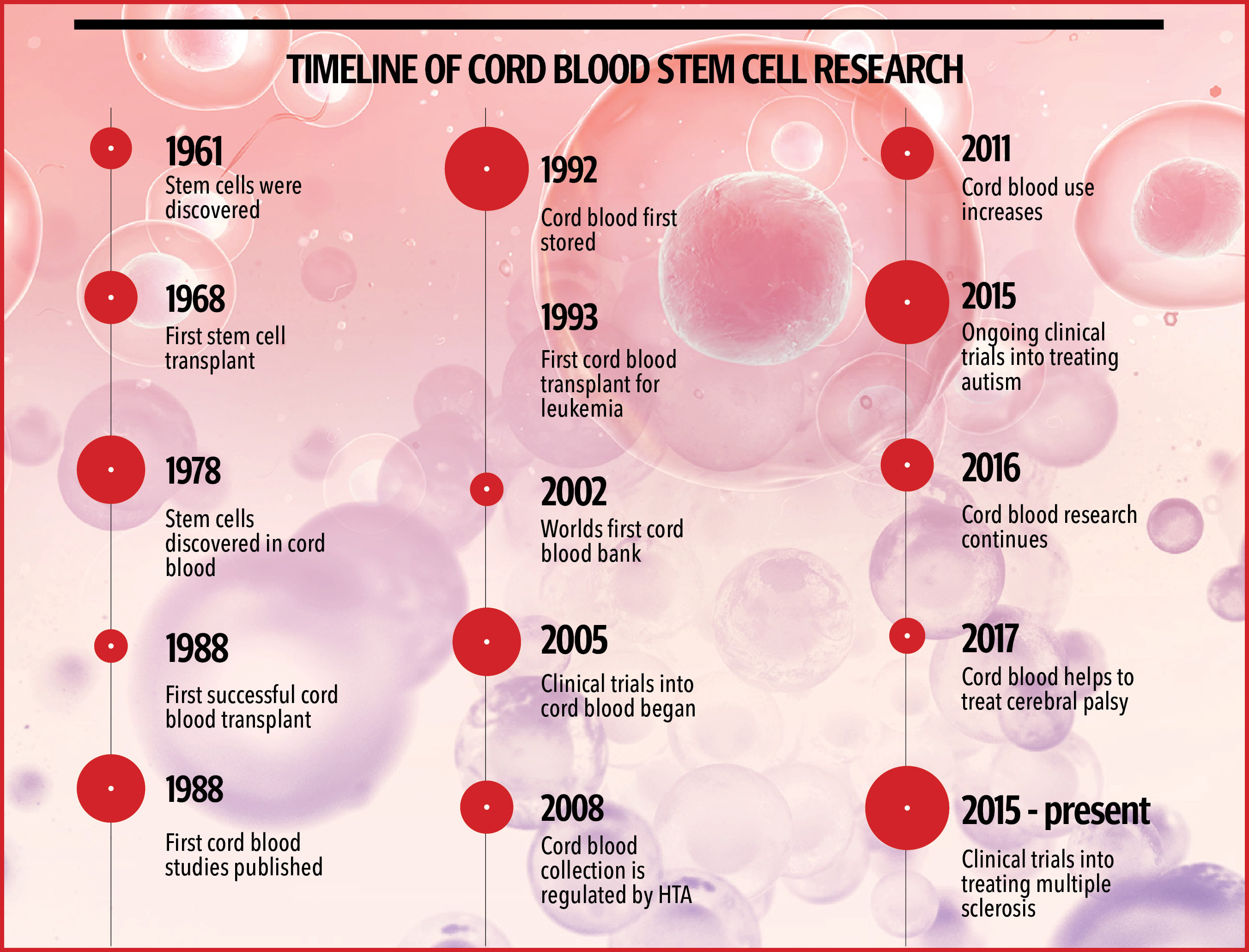
While bone marrow transplants were being conducted in the world as long ago as the 1980s, the first cord blood transplant was done in 1998. “Just like DNA has a lot of data similarly one stem cell can turn into massive stem cells factories, which can help even in curing family members as every one in three is the match in siblings while with parents there is a 25 per cent chance that the cord blood tissue or cells can match,” Dr Baig explained.
The storage process for stem cells and tissues from cord blood is not painful but the procedure can only be done when the child is born. “The stem cells are stored once the baby is out and as soon as the placenta is out it is being clamped before cutting and that is when the blood from the cord can be collected, which has millions of stem cells. These cells are stored through a professional procedure followed internationally and then the cells are transferred and transported to the UK in the kit bag, which they were stored in,” shared Ali, who has been working with the patients directly.
The life of the stem cells before restoring is about seven to eight days with the given condition that they are transferred in a disposable fridge.
To store, a parent can contact any bank which is working in their country and register themselves. “Future Health has two banks, one in Switzerland and one in the UK and cells from the world are transferred according to the distance,” said the regional director.
Once a couple decides to store their child’s stem cells, they have to register themselves and after initial payment of the procedure (a standard sum of £625,) they are registered and a few tests are conducted on the mother. Primary consent is taken from the mother and not the father, and then they are handed over the kit. The storage bank is operating in nearly all major hospitals in the country, where the staff and doctors are also trained in cases where the mother doesn’t allow the team of the bank inside the delivery room. “As soon as labor starts, we are informed and we reach the hospital with our team. In the case C-sections, we are told beforehand,” he said.
The storing of the cells from cord blood doesn’t take a lot of time, after the collection of the blood in the kit, it is labeled and put in a disposable fridge and then transported to the UK. The retrieval process is also as easy as the collection and storage process. Each patient is given a unique ID from which they can contact the bank.
If at any point of time someone needs the cells for treatment, they need to submit a form with the doctor’s letter stating the amount of stem calls needed and after a few verifications from the parents and the hospital, the stem cells are shipped to any part of the world. The whole process takes about three to four days.
The charges for storing of both cord blood cells and tissues is £2075 but if only cells are to be stored the cost is only £1775.
“This cost is one time and then the parents can avail the cells free of cost for 25 years, and there is no transportation cost, storing cost, or any annual cost for it,” he explained. The transportation is done through DHL after a doctor signs and seals the fridge after collecting it.
However, not everyone is able to avail the benefits of stem cell banking. “We do not store cells for patients with HIV, Hepatitis C or Thalassemia major as for them the cells cannot even help,” he added.
The are several stem cell banks in the world where people are able to find donors for themselves or loved ones. There are two types of stem cell banks one is public banks and the others are family banks. There are banks that store stem cells and sell them to patients who need them for treatment while family banks are just for families who are saving the stem cells of their children and can only be used by them.
In want of facilities
Currently, Pakistan is nowhere near ready for treating through stem cells but that doesn’t close the option off for the future. “It is the call of the future and in coming years, many more diseases will be cured through this technology,” said Dr Rubina Hussain, Chairperson of Pakistan for Royal College of Obstetricians and Gynecology-UK.
According to Dr Hussain, several of her patients have begun asking about stem cell banking. “Anyone who can afford should go for it as later on people will regret not getting it saved when there was time, our duty is to inform them or else it’s their decision but we do write on filed for the record that they denied so that after a few years if they need, they can’t blame us for anything,” Dr Hussain added.
In recent times people have been very considerate about their health and vaccination since the pandemic hit and new variants coming every now and then, this has also resulted in an increasing number pf people choosing to store cord blood cells and tissues. “There should be a national level bank in Pakistan to store cells or at facilitate patients and other than that there should be a bone marrow registry in the country as well, which should be affiliated or connected someway to a world bone marrow registry, so that patients can be facilitated well,” said Dr Baig.
Currently, India has eight stem cell banks while Pakistan is still relying on other countries for donors and matches.
“People should be encouraged to donate so that anyone who is in need can be saved,” she added. “It just needs a simple HLA typing where if one matches, their lives can be saved.” “Pakistan should also invest in clinical research as it will be less costly here due to the lower human resource costs and consumable use while even the participants will not be costing much as compared to the UK or USA,” he pointed out how Pakistan is in a better position to start clinical researches on cord blood stem cell.
“When the world was doing first cord blood transplant, Pakistan did its first-ever bone marrow transplant in October 1995, which was conducted by the infamous (late) Dr Tahir Shamsi in Ziauddin hospital, who was treating a patient for AML,” he said.
“People who can afford it are getting their stem cells stored and while the cost of storing is one-off the cost of treatment through stem cells can go into in millions, which makes the whole idea a far-fetched,” said Dr Samina Saleem, head of the gynecology department at a private hospital. She also said that awareness is also the need of the time here where people either who have suffered or have seen someone close in the family dying need to learn and better understand this as a viable but steep costing option.
With the world accepting newer medical approaches, people in Pakistan are still reluctant to accept change. Dr Sarah Feroze who is head of the departmentt at a public hospital shared, “People are opting for storing now but only those who have a family history and who can afford storing them. We educate patients but then again it’s new to the people and there is no work done on this technology on a government level.”
The key to a miracle cure?

After Yumna Aftab’s brother Moiz received his transplant, her family waited with fear to learn if his body would reject the transplant and to see if the cancer would come back. The family was told the time frame for the cancer to return was five years. As that deadline nears, they have finally started to breathe a collective sigh of relief. “He is not just healthy and normally living his life but has also started all his activities back from studying to playing football,” Aftab said.
Still, the process of seeing her brother’s treatment or recovery was arduous. After the transplant, Aftab’s brother’s immune system was weak, his skin tone changed, he lost his hair and lost weight. “[We] didn’t tell our parents about all the physical changes our brother will go through as they would have denied the transplant,” Aftab said. The family had to be extra careful around him while he was recovering to keep him from getting sick.
The aftercare included staying indoors to masking up, as the first year after the transplant was very critical and the risks were very high. The whole procedure was not just challenging for the family but Moiz was also diagnosed with PTSD, anxiety, and depression.
Moiz started therapy and is still recovering but if to be considered how he is saved, it is all just a stroke of luck, where reading a Facebook post led to Moiz being given a fighting chance to live. “People should save their stem cells as it can give 70 per cent opportunity to save lives when God forbid it is needed or else people don’t get matched through public banks that easily,” she said.
The world has not only just evolved in medical science but also is creating options for people to try and save the lives of their loved ones. “Today it seems like a story but it was one of the most difficult times of our lives given the fact Pakistan doesn’t offer such treatments. From finding donors to understanding the treatment, from making travel possible to India to the cost of the treatment, this is not something everyone can do easily,” she shared adding that the transplant cost them around Rs20 million including the stay in India, for all that time and the overall cost of tests. The pre-transplant and post-transplant treatment was also somewhere between Rs 10 to 15 million rupees as even one injection cost was more than Rs 100,000.
The treatment or recovery doesn’t come without a cost. After the transplant, the immune system was just as new, however Moiz’s his skin tone changed and he lost his hair. “From a young, handsome teenager he went to skinny and pale recovering patient.”
“My sister and I didn’t tell our parents about all the physical changes our brother will go through as they would have denied the transplant and after seeing him this way, my father was doubtful of the decision we had made but today, he is healthy, back to normal life and completing his studies in Amsterdam,” she said.
The aftercare for the first year after the treatment was also a challenge as Moiz had to stay indoors and wear mask, as the initial year after the transplant is very critical and possesses higher risks.
The whole procedure was not just challenging for the family but Moiz was also diagnosed with PTSD, anxiety and depression. Since the transplant with the help of therapy, he is recovering but if it is to be considered how he is saved, it is all just a stroke of luck where Yumna’s reading of a Facebook post by chance changed Moiz’s treatment journey. “People should save their stem cells as it can give them 70 per cent higher opportunity to save lives when God forbid it is needed or else people don’t get matched through public banks easily,” she said.
Banking on the future
When his first daughter was born around three and a half years ago, Sunny knew that his life is going to change but had no idea that the journey would be this challenging. The 30-year-old and his wife both are thalassemia minors and his daughter Greesha was a Thalassemia major. They were diagnosed when Greesha was already four months old. “As soon as we were diagnosed, we started visiting doctors to try to save her and the most effective treatment was stem cell transplant but because we never saved the stem cells when she was born, we lost all hope,” said Sunny, who lives in Sukkur and travels to Karachi for blood transfusions every month.
After consulting several doctors when Sunny and his wife didn’t have many options left, the doctor then suggested that the couple plan another baby as the probability of a match through a sibling is higher and the body acceptance of the transplant is also better. “We were given the option to save Greesha so we planned another child and as soon as we conceived, we decided that we will save her stem cells through cord blood. We were lucky enough that the stem cells of my second daughter Amyra who is 16-months-old are a 100 per cent match to Greesha,” he said.
With the given condition of Pakistan’s healthcare and treatment facilities, most of the patients opt for India or USA for transplants. “We plan to go for a transplant when Greesha is at least five years as the success rates are as high as 90 per cent in patients under the age of seven,” said Sunny.
Because of the condition of Pakistan’s healthcare and treatment facilities, the family also opted to go to India for treatment. “The backup plan was to get treatment at the Combined Military Hospital in Rawalpindi but because the hospital can only treat two patients per month for transplants, it could have taken four to five years for Greesha’s operation,” he said.
In India, each hospital is doing about five to seven transplants a week so the experience factor, facilities, and solutions in case of complications are way higher there and moreover, Sunny has a few relatives that can also facilitate him in terms of accommodation and travel. “The treatment facility is similar in US, USA, or India so why not opt for a closer place where language and staying won’t be a big issue,” he said adding that the estimated cost with stay, travel, and all care for the transplant is around Rs10 million.
The technology is new to Pakistan, people are unaware also it is expensive for a country where the inflation rate is high but still many are opting for it. “I didn’t have any medical history but I myself had an interest in medical science so I searched and found Future Health and got tcord blood stored for my first child back in July 2018,” said Sharjeel Salman, who has stored cells of both of his children. The way he sees it, storing stem cells is no different than freezing eggs or sperm -- new technologies that are changing people’s lives for the better.
Another parent, Ayesha Siddiqui, stored stem cells for her two-year-old son because both her father and mother-in-law have had cancer. “I thought that stem cells might come in handy in the future, I hope no one needs them but it’s better to be precautious,” she said. When Siddique was pregnant with her first child, she didn’t take the idea of storing stem cells seriously. But since learning it can help cure diabetes, autism, and other diseases, she has been encouraging others to do it. “I even told my sister who lives in Australia to opt for stem cell storing,” she said.
Some parents remain skeptical about how stem cells are stored. “We were curious to know if the cells are being stored are thrown away or what, so we kept a check and balance and confirmed from a few people whom we knew about the legitimacy of the bank,” said Anum Baig.
Baig’s brother stored cells for his child through an agent who lacked many necessary documents. Baig opted to store cells at Future Health; She is happy about that because, with the information they got from her blood, the family was able to diagnose her minor health problems more easily. “My daughter was lactose intolerant and we would have never known this until the tests were done so it was a blessing for me,” she added.